9/20일에 골수천자가 임기표 원장님 병원에서 있다고 해서 자료를 찾아 봤습니다.
첨부파일도 열어보세욤.
결국, post. illiac crest에서 하는 것이 좋겠습니다.
저는 실제로 골수천자를 하는 것을 본적이 있는데요.
감염을 막는 것이 중요해 보였습니다.
골수검사
【실시부위】
1) 후장골능(posterior iliac crest) : 모든 연령층에서 골수생검과 천자
2) 전장골능(anterior iliac crest) : 유아와 소아, 비대증 환자
3) 흉골(sternum) : 15세 이하에서는 실시하지 않고 어른에서 천자만 가능
4) 경골(tibia) : 18개월 미만의 유아에서 실시하며 보통 골수천자만 시행
【준비물】
골수천자만을 위해서는 Illinois needle가 사용되기도 하지만, 통상 Jamshidi Bone Marrow Biopsy/ Aspiration needle로 천자와 생검을 실시한다. 고정액으로는 10% formalin을 사용하고 각종 세포화학검사(cytochemistry)를 실시할 경우에는 그에 해당하는 고정액을 준비하여야 한다. 염색체검사나 세포배양이 필요할 경우는 보존제가 첨가안된(preservative-free) heparin tube도 준비한다.
그림 14. 골수천자용 Illinois Needle(왼쪽)과 Jamshidi BM Aspiration/Biopsy Needle(오른쪽)
골수천자 도말과 생검조직 표본은 각각 Wright 염색과 H&E 염색을 시행하였다.
- 시행해서는 안되는 경우 : 중증 혈우병(hemophilia) 환자에서는 응고인자를 보충해주고 실시하여야 하며, 혈소판감소증일 경우는 혈소판 수혈 없이도 대부분 골수검사를 시행할 수 있다.
【적응증】
① 임상적으로 혈액질환이 의심되고 임파절, 비장 및 간이 커져 있을 경우
② 말초혈액소견이 골수이형성증후군 또는 백혈병을 의심케 하는 경우
③ 원인을 알 수 없는 심한 빈혈, 혈소판 감소, 백혈구 감소가 있을 경우
④ 뼈의 방사선 소견에서 혈액질환이 의심되거나
⑤ 암의 전이여부(metastasis)를 확인하고자 할 경우
⑥ 육아종(granuloma)의 세균학적 또는 병리조직학적 검사를 목적으로
⑦ Storage disease나 골질환의 진단
⑧ 빈혈, 백혈병 등의 치료효과와 예후 판정
⑨ 다발성골수종의 진단이나 면역글로불린의 이상이 있는 경우
⑩ 철결핍성빈혈, 거구성빈혈 등 혈액질환의 추적검사, 골수배양, 세포유전학적검사
- 검사비용 (미국 W/U 및 국내 의료보험 수가 비교, 1991)
| Bone marrow aspiration and biopsy = $550 (국내 36,680원) Cytogenetic analysis = $685 (국내 70,270원) CBC / Platelets / WBC differential = $ 49 (국내 4,960원) Chest X-Ray = $150 |
Posterior/Anterior Iliac Crest
A marrow biopsy is generally performed before aspiration sampling due to the fact the biopsy technique induces elevated thromboplastic substances. The consequence of this is a reduction in the effectiveness of an aspiration sampling. However, as many clinical requests are for an aspiration sample only, this technique is described first.5,8,9
- The patient is placed in the lateral decubitus position, with the top leg flexed and the lower leg straight.
- Palpate the iliac crest, and mark the preferred sampling site with a pen.
- Aseptic technique is employed, including sterile gloves and gown.
- The site is prepared with an antiseptic (eg, povidone-iodine or chlorhexidine gluconate), scrubbed, and draped, exposing only the site to be sampled.
- The skin and the underlying tissue to the periosteum are infiltrated with a local anesthetic (eg, approximately 10 mL of 1% Xylocaine [lidocaine]). A 10-mL syringe with a 25-gauge needle is used to inject an initial 0.5 mL directly under the skin, raising a wheal. A 22-gauge needle is used to penetrate deeper into the subcutaneous tissue and the underlying periosteum, an area roughly 1 cm in diameter.
- Adequacy of the anesthesia is tested by gently prodding the periosteum with the tip of the needle and questioning the patient for any painful sensation. It is important to be aware of changes in the patient's comfort level throughout the procedure to not only decrease the patient's anxiety level, but to minimize movements that may affect the efficacy of the procedure. Having a family member present may help to alleviate the patient's anxiety. To ensure sufficient pain control is being managed well, the person performing the procedure should talk to the patient, discuss the steps taken throughout the process, and listen to the manner as well as the content of the patient's response.
- A skin incision is made with a small surgical blade, through which the bone marrow aspiration needle, with a stylet locked in place, is inserted.
- Once the needle contacts the bone, it is advanced by slowly rotating clockwise and counterclockwise until the cortical bone is penetrated and the marrow cavity is entered. Contact with the marrow cavity is usually noted by a sudden reduction in pressure. The depth of the penetration should not extend beyond an initial 1 cm.
- Once within the marrow cavity, the stylet is removed. Using a 20 mL syringe, approximately 0.3 mL of bone marrow is aspirated. A volume greater than 0.3 mL may dilute the sample with peripheral blood and thus is not recommended. The material collected for bone marrow slides is generally not mixed with an anticoagulant, and it is processed immediately by a technologist; this avoids any cellular morphologic artifacts. If there is to be a delay in slide preparation, place the sample in an EDTA (ethylenediaminetetraacetic acid) anticoagulant-containing tube, preferably a pediatric-sized tube to avoid exposure to excess anticoagulant.
- If additional marrow is needed for ancillary studies, subsequent specimens are obtained by attaching a separate syringe, collecting 5 mL at a time. The samples are then transferred into an anticoagulant-containing tube that is appropriate to the requested study: heparin for cytogenetic analysis; either heparin or EDTA for immunophenotyping; formalin for a Cytoblock preparation; and, gluaraldehyde for ultrastructural examination.
- The marrow needle is removed, and pressure is applied to the aspiration site with gauze until any bleeding has stopped (see Postprocedure Care).
- Once the aspiration is completed, the specimen is processed by the hematopathology technician.
Any of several needle models can be utilized; however, the Jamshidi needle is considered the most popular. This disposable needle is tapered at the distal end to help retain the specimen for improved extraction.
- Patient preparation is to be followed in the manner previously described for bone marrow aspiration.
- The needle, with stylet locked in place, is held with the palm and index finger and repositioned so that a new insertion site is created for biopsy sampling. Once the needle touches the bone surface, the stylet is removed.
- Using firm pressure, slowly rotate the needle in an alternating clockwise-counterclockwise motion, and advance it into the bone marrow cavity to obtain an adequate bone marrow specimen measuring approximately 1.6-3 cm in length.
- Rotate the needle along its axis to help loosen the sample, pull back approximately 2-3 mm, and advance the needle again slightly, at a different angle, to help secure the specimen.
- Following this procedure, slowly pull the needle out, while rotating in an alternating clockwise and counterclockwise motion.
- Remove the specimen from the needle and introduce a probe through the distal cutting end. If the aspirate was unsuccessful (ie, a "dry tap"), the core biopsy may be used to make touch preparations (see Slide Preparation). This must be performed before placing the specimen in formalin.
- Place the specimen in formalin solution for histologic processing.
- The marrow needle is removed, and pressure is applied to the site with gauze until any bleeding has stopped (see Postprocedure Care).

1: Patient position (superior posterior iliac crest).

Bone marrow tray

Skin preparation.

Site preparation.

: Local anesthetic injection.

Aspiration needle placement.

Bone marrow aspiration.
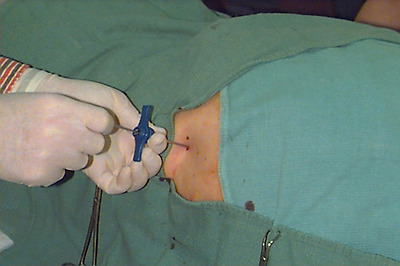
Bone marrow biopsy. Jamshidi needle placement.
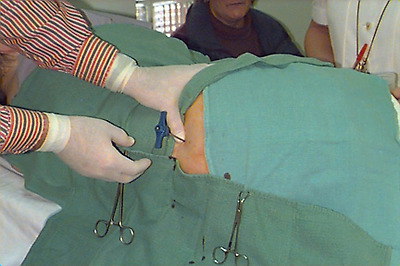
Bone marrow biopsy. Jamshidi needle placement.

Bone marrow biopsy specimen.

Bone marrow biopsy specimen.


