mri로 신경과 근육의 진단에 대한 40페이지 논문
MR neurography라는 새로운 진단영역에 관한 논문이다.
꼭 기억해야 한다.
mri 사진보다 더 중요한 것은 neurologic exam에 의한 symptom, sign임을
MR neurography and muscle MR imaging for image diagnosis of disorders affecting the peripheral nerves and musculature
![]() MR neurography and muscle MR imaging 말초신경과 근육.pdf
MR neurography and muscle MR imaging 말초신경과 근육.pdf
Medical imaging, including MR imaging [1], is playing an increasingly important role in the diagnosis of disorders affecting the peripheral nerves and muscles [2,3]. In the past, the practical application of MR imaging of nerves has been limited by technical difficulties in obtaining good image contrast to help distinguish nerve from neighboring tissues [4–9]. By comparison, the limited capabilities of ultrasound [10] for nerve identification have seemed useful. Recently, however, advances and enhancements of MR imaging techniques have transformed the evaluation of a variety of conditions that have posed diagnostic challenges in the past.
The term MR neurography is used to describe the new techniques for nerve imaging that greatly improve the reliability of identification of peripheral nerves in images and often make it possible to generate tissue specific images of nerves analogous to angiograms. These images enable the physician to examine the peripheral nerve for anatomic abnormalities. A series of discoveries in basic MR science beginning in 1992 has led to the establishment of MR neurography as a distinct area of imaging [11,12].
The technique has now been applied in thousands of clinical cases. A series of publications cover the basic science [13–15], imaging science [16,17], and clinical application [18–23] of the technique. Large, well-controlled formal outcome trials [24,25] have established, at least in some settings, that MR neurography can be more reliable than electrodiagnostic studies in localizing peripheral nerve disorders and in guiding treatment planning.
The referring physician should be aware of some of the technical aspects of MR nerve imaging. Many radiologists have limited experience with nerve imaging, and many imaging centers are not adequately equipped to carry out these studies successfully. It is important for the referring physician to have a clear idea of how a useful high-quality nerve image should appear.
Awareness of some of the general technical aspects of the nerve imaging process can help the referring physician understand and address image quality problems that can arise as this new technique is introduced in a community.
중간 생략
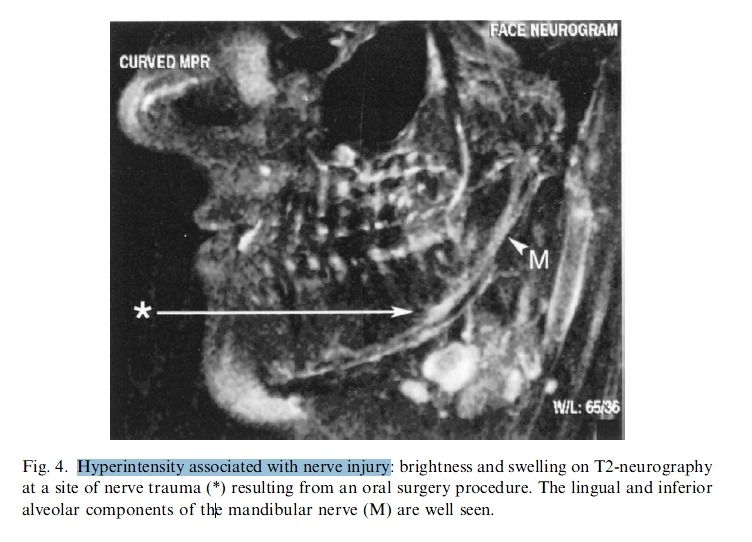
Image appearance of nerve pathologies
MR neurography makes it possible to view images that depict many types of nerve pathologies which previously could only be inferred (Fig. 4). Nerve swelling, including edema at the fascicular level, can often be seen (Fig. 5). Mechanical deviations in the physical course of a nerve can indicate entrapment or adhesions (see Fig. 2), and hyperintensity associated with nerve injury may be appreciated in nerves affected so severely as to be associated with significant motor deficits. Physical discontinuities in nerve and the development of traumatic neuromas may be readily appreciated. In
hereditary neuropathies, disordered distribution of interfascicular lipid can be detected.
Fig. 2. Assembly of raw images by maximum intensity projection (MIP). This process can greatly enhance the diagnostic value of the images. (A) Series of four oblique coronal image sections, each showing portions of the exiting cervical spinal nerves and proximal brachial plexus. Isolated segments of nerve elements appear at various locations, and some are difficult to identify reliably. (B) An overlay MIP made possible because the nerves are among the brightest elements in the image. It is easy to match the dorsal root ganglia (d) with the cervical spinal nerves because of the appearance of physical continuity. Nerve hyperintensity (h) associated with motor symptoms is readily appreciated in the right C6 cervical spinal nerve because the lower intensity of all the other elements is easily seen. Evidence of downward distortion of the right C7 and C8 cervical spinal nerves (s) by an enlarged scalene muscle is also readily seen because of the assembled view of the entire proximal plexus bilaterally.
MR neurography extends the capabilities of diagnostic imaging to a wide variety of pathologies affecting the peripheral nerves [3]. The principles of localization and characterization of lesions in the nervous system are well known. The lack of use of imaging for peripheral nerves in the past reflects only the longstanding inability of existing imaging technology to provide those images. CT scanning advanced the diagnosis of intracranial lesions relative to pneumoencephalography and angiography because of the improved detail of localization and extent of identification of lesion type. MR imaging, at a minimum, extended the capabilities of localization to include accurate views of the contents of the posterior fossa while generally improving the quality of lesion characterization throughout the body. MR neurography now plays a similar role with regard to the peripheral nervous system [22,23].
The indications for MR neurography include visualization of the distal spinal roots and spinal nerves and plexuses for the effects of degenerative disease, entrapments, adhesions, and the effects of trauma. In addition, this technique permits reliable identification and precise localization of nerve tumors as small as 2 mm in diameter. In problematic conditions such as TOS, MR neurography allows the diagnostic sorting of this condition into a series of distinct and reliably
diagnosed types of specific pathology. Sorting by accurate diagnosis before treatment is already beginning help in optimizing both the details of treatment planning and treatment.
Entrapments and compressions
Sciatica of nondisc origin
Lumbar and sacral spinal nerves
Persistent sciatica not responsive to conservative measures is one of the most common indications for MR imaging. Of 1.2 million MR imaging scans obtained each year for back pain and sciatica, however, only about one in four scans demonstrates a surgically treatable lesion. Among patients treated with surgery, a significant fraction fail to improve; in many cases this lack of improvement results from misdiagnosis before surgery, and in other cases it results from inadequacies of the surgery. For all of these reasons, neurologists and neurosurgeons are commonly asked to evaluate patients with persisting sciatica who do not have a herniated disc or whose surgery has failed.
- 보존적인 치료에 반응하지 않는 지속적인 좌골신경통은 MR imaging의 가장 흔한 적응증.
- 하지만 4명중 1명만 수술적으로 적합한 lesion이 관찰됨.
- 수술을 받은 환자중에서 증상개선이 안되는 경우는 정확한 진단의 실수가 많음. 그래서 많은 신경과, 신경수술의사는 지속적인 좌골신경통을 정확하게 진단하려 애씀.
Successful treatment of persistent radiculopathy after lumbar spine surgery requires effective diagnostic categorization of the causes. Electrodiagnostic studies often can demonstrate only that the radiculopathy present before surgery is still detectable.
Use of image-based diagnosis can help further differentiate among the cases that should be directed toward reoperation, radiofrequency neurolysis, or medical treatments directed at inflammation. Direct imaging of the lumbar/sacral spinal nerves and the proximal sciatic nerve with neurographic techniques can help resolve the diagnosis in many of these patients [44]. The lumbar spinal nerves, ganglia, and the proximal sciatic nerve can be imaged reliably and effectively. In general only the larger, more proximal lumbar nerves can be imaged reliably at present; however, there is no strict physical limit on the size of nerves that can be imaged under optimal conditions.
Foraminal pathology.
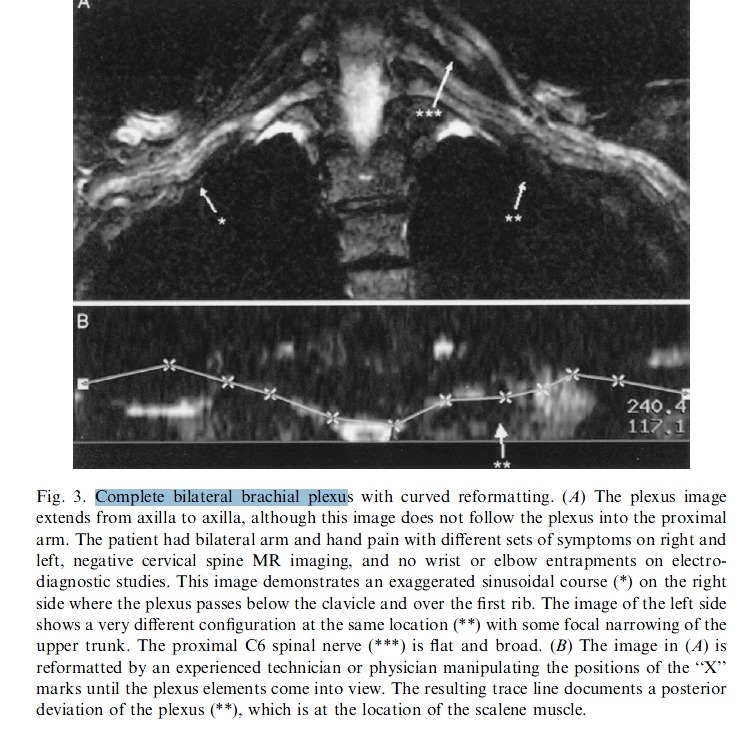
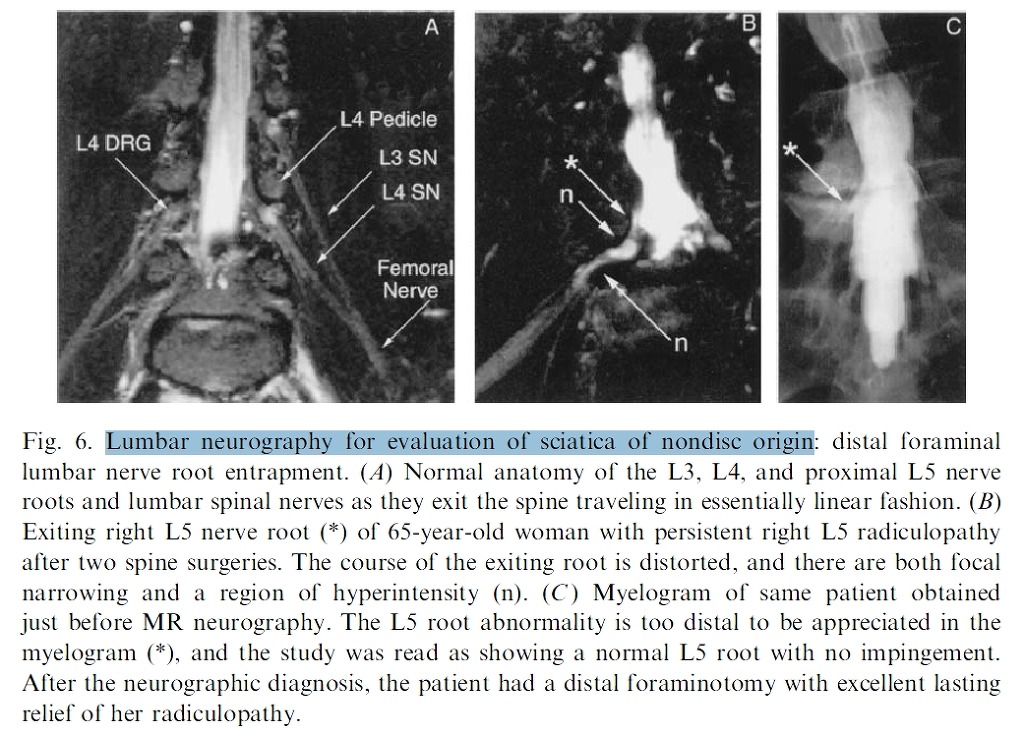
The normal course of the lumbar spinal nerves is in a smooth straight line (Fig. 6A). In patients with a nondiagnostic MR study and myelogram, MR neurography can demonstrate distortions of the course of the exiting nerve in the distal foramen, which are readily susceptible to surgical correction (Fig. 6B,C). MR neurography is particularly helpful for imaging foraminal spinal disease in the presence of scoliosis because the three-dimensional aspects of the imaging tend to resolve some of the ambiguities that may otherwise make diagnosis challenging.
Even when myelography is capable of demonstrating a nerve root cutoff, a MR neurogram can provide considerable additional information. The full length of the foraminal impingement requiring treatment can be easily appreciated, and this visualization can avoid an incomplete foraminotomy. In addition, the ability of MR neurography to demonstrate hyperintensity in the lumbar root adjacent to the impingement helps confirm the significance of the impingement.
Postsurgical radiculopathy.
MR neurography is the study of choice for evaluating persistent, exacerbated, or altered radiculopathy after lumbar
spinal surgery. It allows clear differentiation of several different causes of this problem and identifies cases that are best treated by reoperation, by allowing additional time to elapse, or by referral for electronic stimulators or other treatments for chronic, irremediable pain. In a number of common situations, MR neurography can provide a specific diagnosis determining treatment by revealing pathology that cannot be detected by any other methodology.
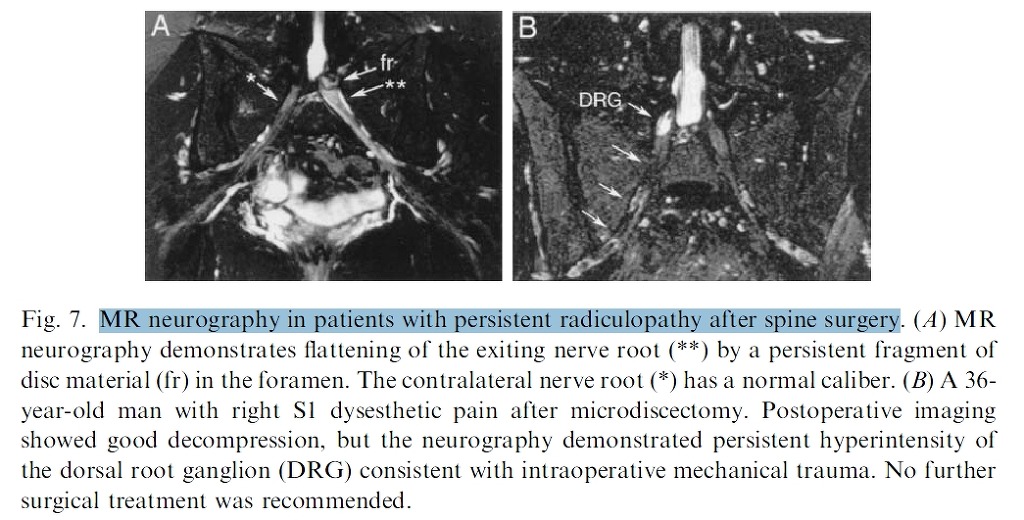
Postoperative hyperintensity in the ganglion can be connected with a specific anatomic feature not adequately treated by the surgery, such as a persistent bone spur. In other cases, MR neurography has demonstrated impaction of a disk fragment in the distal foramen compressing the root (Fig. 7A), which is treatable by reoperation. The study may also show hyperintensity only in the ganglion with no associated mechanical impingement.
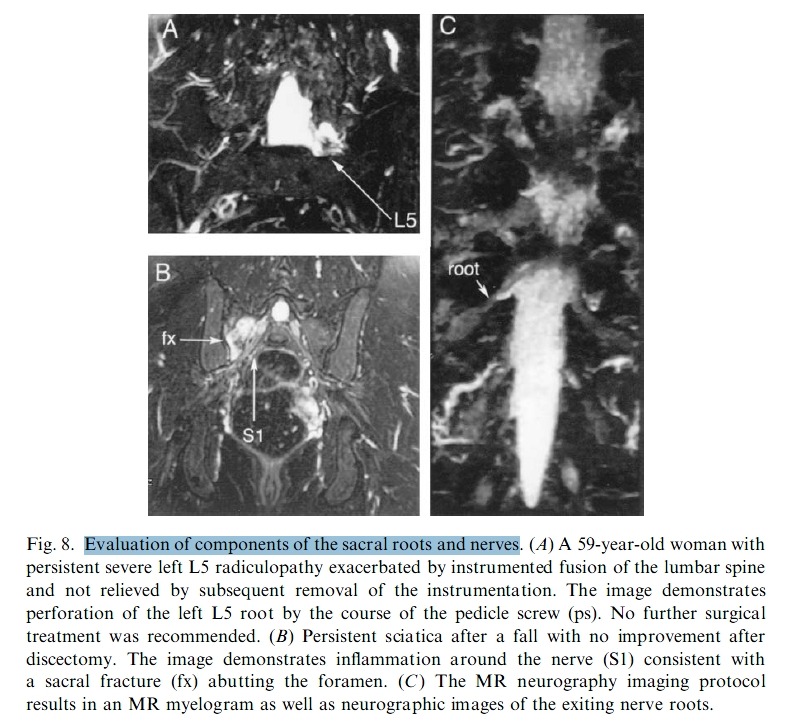
This finding would be consistent with intraoperative mechanical trauma to the nerve (Fig. 7B), for which there is no urgical treatment. The imagable effects of mechanical trauma on nerve roots are varied. One cause of trauma is mechanical distortion of the shape of the root, as in Fig. 8A, which depicts a root penetrated by a pedicle screw. Alternately, there may be nerve pain associated with inflammation nearby, as in the radiculopathy associated with a sacral fracture depicted in Fig. 8B. Because of the myelographic effect present in lumbar MR neurography (Fig. 8C), it is possible to assess the effects of stenosis and disk herniation as well as details about nerve pathology.
Another diagnosis made possible by neurography in lumbar monoradiculitis, a condition that is easily mistaken for a herniated disk syndrome if any disk abnormality happens to be seen in the patient’s MR image.
Piriformis syndrome
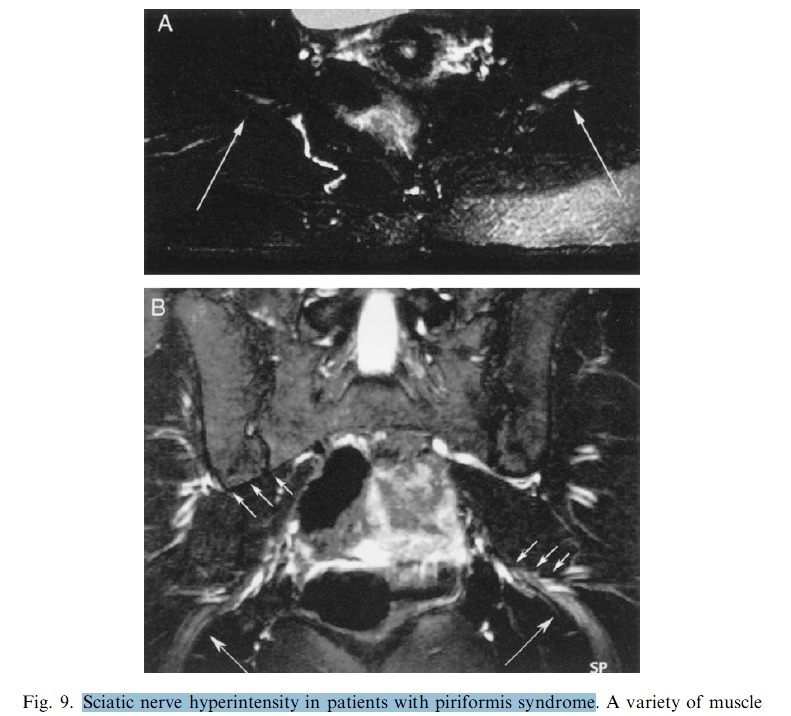
Imaging is increasingly capable of helping provide a reliable for diagnosis of piriformis syndromes [45]; in some patients with severe symptoms, hyperintensity or shape changes are seen (Fig. 9). When MR neurography can identify specific focal entrapments, open MR imaging can guide surgical procedures with limited surgical exposure to approach the site of the abnormality for decompression or release of adhesions.
It is straightforward to use a T1 image to obtain volume and shape assessments of the piriformis muscles to assess asymmetries reflecting either hypertrophy or atrophy. In addition, these images can readily demonstrate variant courses of the distal lumbosacral plexus that may actually pass through the muscle. This course is an important piece of preoperative information, because surgical strategies aimed at extensive muscle removal may be modified to reduce the risk of nerve injury. A correlated neurographic image can confirm the identity of the structure as a nerve. Scanning of the distal lumbosacral spinal nerves, lumbosacral plexus, and sciatic nerve may also reveal tumors as the cause of sciatic distribution pain.
Fig. 9. Sciatic nerve hyperintensity in patients with piriformis syndrome. A variety of muscle and nerve abnormalities can be observed in the pelvis in patients with sciatica of nonspinal origin. In some cases, nerve fascicle swelling and hyperintensity can be observed. (A) Axial view just below the exit from the sciatic notch where the sciatic nerves (arrows) lie over the surface of the ischium with the piriformis muscle immediately posterior. (B) Coronal view demonstrating a linear fascicle pattern in the right sciatic nerve (right arrow) with hyperintensity and loss of fascicle pattern in the left sciatic nerve (left arrow). These arrows indicate the curve of the sciatic nerve as it turns downwards after exiting the sciatic notch. The three arrows on the right indicate the attachment of the piriformis muscle on the sacrum and across the sacroiliac joint. The three arrows on the left indicate the inferior surface of the piriformis muscle where the sciatic nerve and some gluteal vessels emerge from underneath it.
Thoracic outlet syndromes
TOSs have been problematic diagnostically because of the difficulty of obtaining surgically useful localization of sites of brachial plexus compression. Indeed, the limitations in the quality of diagnostic techniques have led to ongoing disagreements about the very existence of this class of nerve entrapment syndromes.
In part these problems arise because of the difficulty in placing diagnostic electrodes for electrophysiologic studies in this region. Also, because many cases of TOS result from nerve compression by the scalene muscle, patients often present with pain elicited by motions such as arm raising but do not have sufficient motor symptoms to produce an abnormal electromyography.
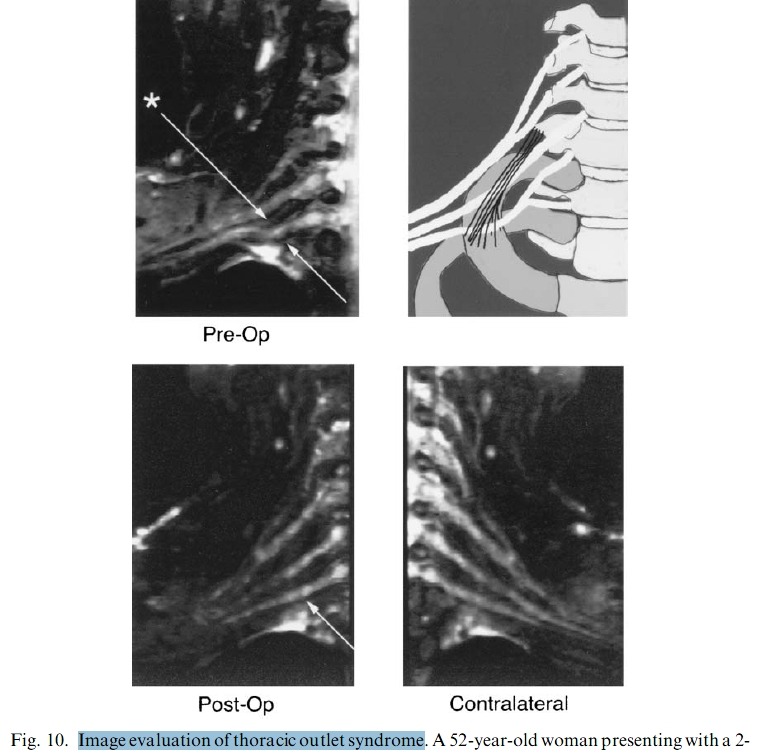
Finally, the diagnosis of TOS is greatly complicated because the term describes a variety of diverse underlying pathologic conditions that have in common only the fact that they affect some part of the brachial plexus. MR neurography has shown promising capabilities for discriminating among several different types of TOS lesions and in many cases can depict well delineated and readily treatable specific pathologic conditions [32,33]. Anterior scalene muscle syndromes can be detected by observing asymmetries in the course of brachial plexus elements as they traverse the scalene border. Entrapment by fibrous bands in the region can also have a distinct appearance in the form of kinking of the elements (Fig. 10).
Fig. 10. Image evaluation of thoracic outlet syndrome. A52-year-old woman presenting with a 2-year history of pain in the right fourth and fifth digits and negative electromyography/nerve conduction velocity (NCV) of the ulnar nerve at elbow and wrist, who has no cervical disc disease. (A) Preoperative neurography shows a kink distorting the course of the lower trunk of the brachial plexus. (B) The diagram identifies the anatomy and shows a fibrous band extending from the C7
transverse process to the first rib that causes the image finding. After resection of the anterior scalene using a supraclavicular approach and neurolysis of the lower trunk, the patient experienced complete relief of right hand and arm symptoms, now maintained at nearly 2 years’ follow-up. (C) Postoperative and (D) contralateral images from the same patient show the mechanical result of the surgery in restoring normal anatomy.
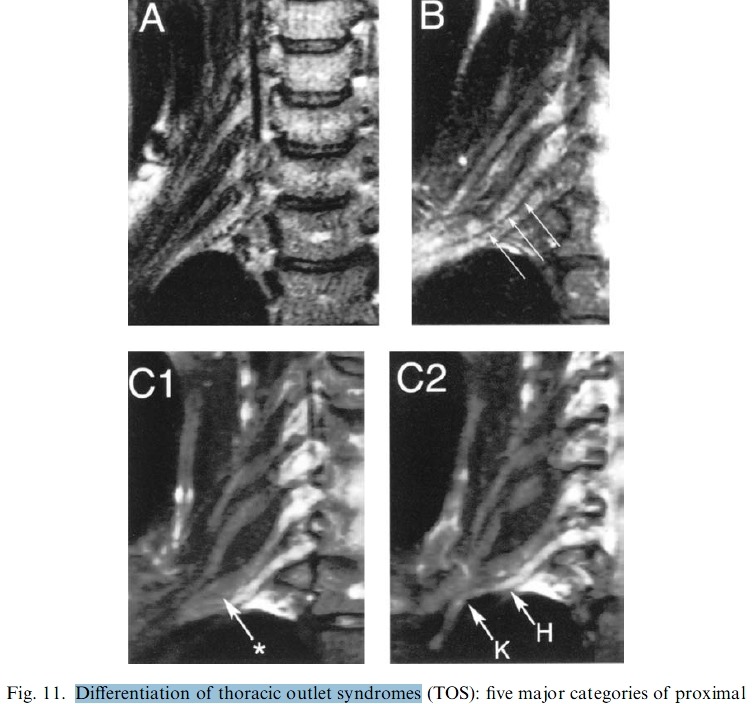
In a hypertrophied scalene muscle with no fibrous band, the distortion of the course of the plexus is smoother but nonetheless can be readily distinguished from the normal straight course through the region (Fig. 11). Surgical treatment of such proximal pathology in the region of the anterior scalene muscle may be more effectively treated by a supraclavicular approach.
Fig. 11. Differentiation of thoracic outlet syndromes (TOS): five major categories of proximal and midplexus TOS disease based on imaging characteristics. (A) In the normal plexus, the cervical spinal nerves and trunks of the brachial plexus follow a straight trajectory with even spacing. (B) Scalene syndrome is demonstrated by a gentle deformation of the course of the nerve elements and loss of space between them. In patients with pain only, there is usually no nerve hyperintensity. (C1) Distortion of the shape of the C7 element (*) associated with a severe TOS case. (C2) A more anterior image plane in the same patient showing both a sharp kink (K) in the course of the lower trunk associated with a fibrous band and nerve hyperintensity (H) consistent with lower trunk motor symptoms.
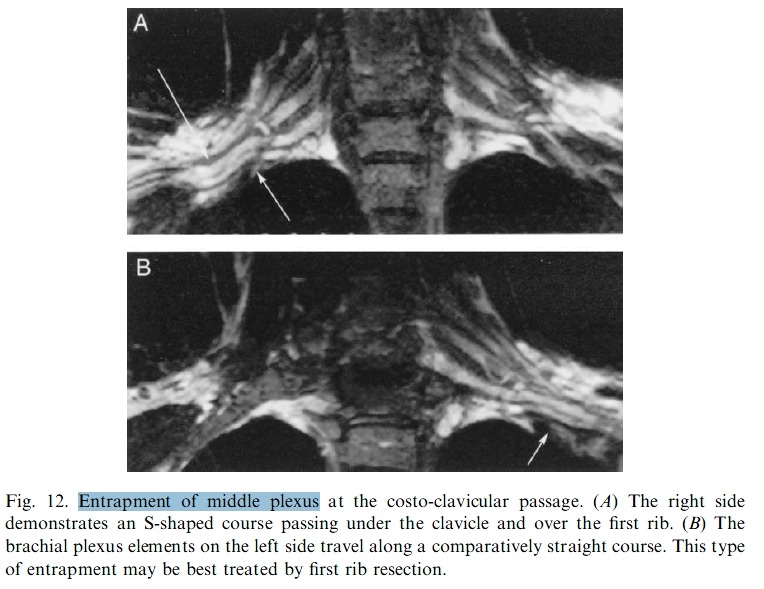
A variety of types of more distal pathology can also be distinguished. Passage of the plexus over the first rib can demonstrate a distortion associated with entrapment at the level of the clavicle (Fig. 12). Patients with this sort of entrapment are often best managed with first rib resection when conservative management fails.
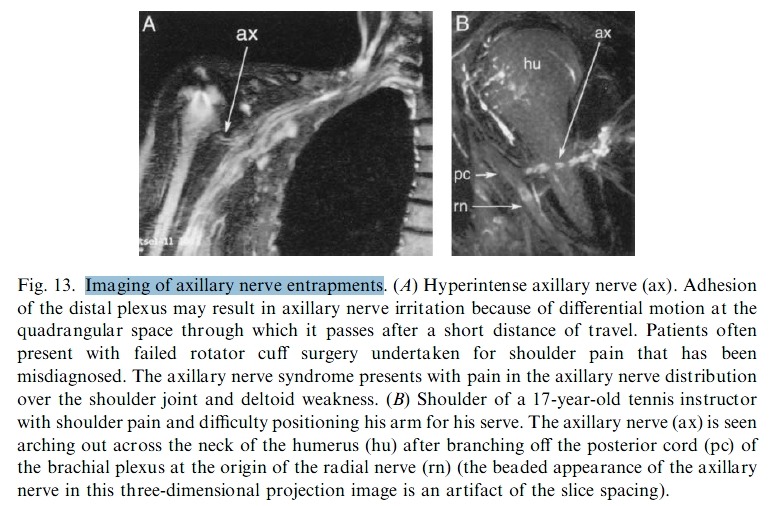
In addition, brachial plexus entrapments in the axillary region can be defined as distinct entities (Fig. 13). On physical examination, these patients may have tenderness and Tinel’s sign in the axilla. Entrapment in this region may be a consequence of chronic degenerative change but may also occur as a complication of breast surgery or shoulder surgery. A related problem that has been difficult to document properly in the past is axillary nerve entrapment. These patients typically present with shoulder pain and deltoid weakness. Unfortunately, this set of findings is sometimes mistaken for the consequence of a rotator cuff tear, leading to unnecessary and unsuccessful rotator cuff surgery.
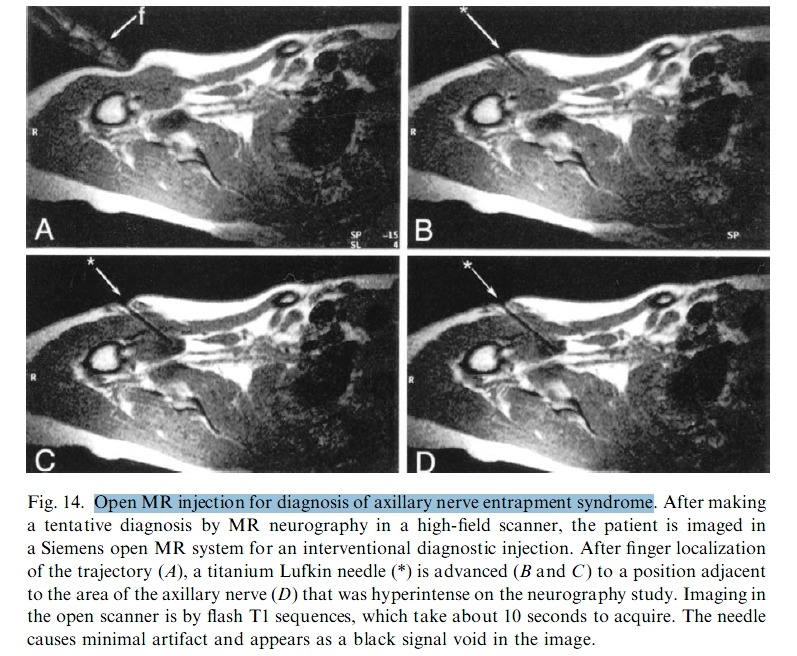
Abnormalities in the axillary nerve detected in an MR neurography study can be confirmed by proceeding to a nerve block at the location of the apparent abnormality. Such a block may be performed in an open MR scanner in which an image plane that duplicates the anatomy of thediagnostic MR neurography study can be used to guide needle placement
(Fig. 14).
If the pathology can be confirmed, it is often possible to treat the axillary nerve entrapment with a transaxillary neurolysis, which is a relatively simple procedure with rapid postoperative recovery. In addition to surgically treatable entrapments, MR neurography is also helpful in identifying complaints attributable to the nerve inflammations.
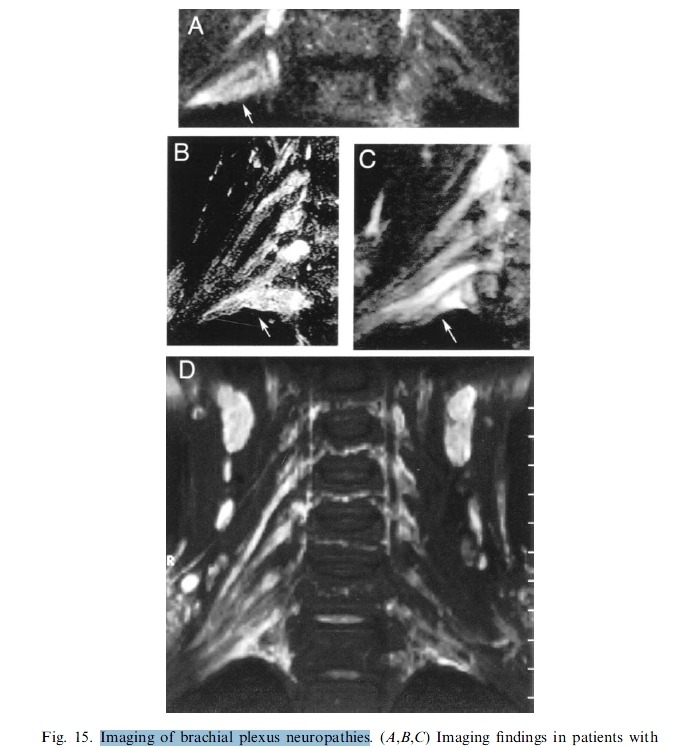
These patients often present with painless hand atrophy, with no associated sensory abnormality. This presentation has sometimes been termed a Gilliatt-Sumner hand syndrome. Brachial plexus elements appear bright and swollen but demonstrate no distinct evidence of impingement (Fig. 15).
Fig. 15. Imaging of brachial plexus neuropathies. (A,B,C) Imaging findings in patients with painless pure motor weakness of hand intrinsics with no sensory findings (Gilliatt-Sumner hand syndrome). There is hyperintensity and swelling in the elements of the lower trunk without mechanical deformation or other evidence of mechanical entrapment. Surgical treatment is unlikely to be effective, and an inflammatory or vascular cause is suspected. (D) Diffuse plexitis
of unclear origin in the right brachial plexus. Management is nonsurgical, and physical therapy may not be helpful.
MR neurography is also helpful when it demonstrates a completely normal course and caliber for all nerve elements that are under suspicion. With such findings, it is possible to take a firm stance against surgical treatment of the hand, arm, or shoulder problems that may have been tentatively attributed to a TOS. The information gained by MR neurography has proven helpful because it permits the treatment of TOS with more limited surgeries directed at individual pathologic conditions. Operations such as supraclavicular scalenotomy or transaxillary neurolysis are less invasive and may have lower surgical risks than transaxillary first rib resection. Use of MR neurography may make it possible to reserve the use of first rib resection for the small number of patients in whom the less-invasive operations are not appropriate.
Fig. 16. Movement of the median nerve with wrist flexion: images of the same location in the hand in the same individual. (A) In flexion the median nerve (mn) at the wrist located near the palmar aspect of the carpal tunnel with the tendons (te) posterior to it. (B) In extension the median nerve is posterior to the tendon in this image.
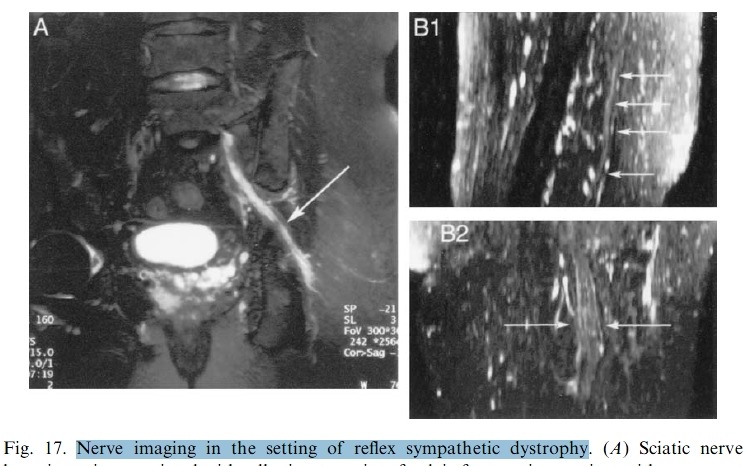
Fig. 17. Nerve imaging in the setting of reflex sympathetic dystrophy. (A) Sciatic nerve hyperintensity associated with adhesion to a site of pelvic fracture in a patient with new-onset reflex sympathetic dystrophy. The symptoms of reflex sympathetic dystrophy resolved after nerve-release surgery. (B) Deformation in the shape of the sciatic nerve at a site of prior trauma and failed surgical exploration. (B1) Reconstruction in the sagittal plane shows a flattened sciatic nerve with an irregular course instead of the expected straight, smooth course. (B2) In the coronal view the sciatic nerve is broad and flat. The two images together show the severe mechanical distortion of the nerve at this site of adhesion. After 4 years of failed intensive pain management, the symptoms were relieved by nerve-release surgery.
Fig. 18. Confirmation of total nerve disruption in trauma. (A) The right brachial plexus of a 15-year-old with flail arm, 2 months after a motorcycle accident. The image demonstrates gross discontinuities in the upper plexus elements (ue), meningoceles proximally (me), and bright swollen nerve trunks (st). (B) Disconnected and retracted lower trunk (lt) in traumatic injury of brachial plexus.
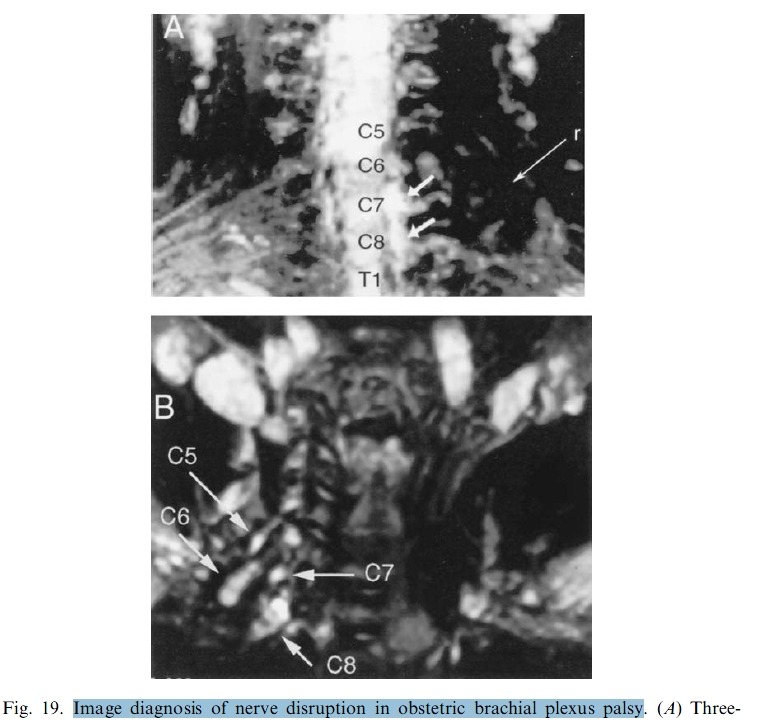
Fig. 19. Image diagnosis of nerve disruption in obstetric brachial plexus palsy. (A) Three month-old with complete flail arm. Image demonstrates absence of plexus elements in area of trunks. A hypointense round (r) abnormality proved to be a mass of disrupted, scarred scalene muscle partially incorporating shards of nerve remnants. (B) Six-month-old child with persistent upper trunk paresis. Imaging confirmed ball neuromas at C5 and C6 demonstrating
complete disruption of upper trunk elements.