퇴행화는 MRI상 어떻게 보이는가?
rupture of the interspinous ligament(s),
neoarthrosis of the interspinous space with perispinous cyst formation,
posterior spinal facet (zygapophyseal joint) arthrosis,
related central spinal canal, lateral recess (subarticular zone) and neural foramen stenosis,
posterior element alterations associated with various forms of spondylolisthesis, and
perispinal muscle rupture/degeneration.
panic bird..
Abstract
A review of the imaging features of normal and degenerative anatomy of the spine on medical imaging studies shows features that have
been largely overlooked or poorly understood by the imaging community in recent years. The imaging methods reviewed included computed tomography (CT) with multiplanar reconstructions and magnetic resonance imaging (MRI).
A routine part of the MRI examination included fat-suppressed T2 weighted fast-spin- or turbo-spin-echo acquisitions. As compared to the normal features in asymptomatic volunteers, alterations in the observed CT/MRI morphology and MR signal characteristics were sought in symptomatic individuals.
Findings in symptomatic subjects which departed from the normal anatomic features of the posterior spinal elements in asymptomatic
volunteers included:
rupture of the interspinous ligament(s),
neoarthrosis of the interspinous space with perispinous cyst formation,
posterior spinal facet (zygapophyseal joint) arthrosis,
related central spinal canal, lateral recess (subarticular zone) and neural foramen stenosis,
posterior element alterations associated with various forms of spondylolisthesis, and
perispinal muscle rupture/degeneration.
These findings indicate that the posterior elements are major locations of degenerative spinal and perispinal disease that may accompany or even precede degenerative disc disease. Although not as yet proven as a reliable source of patient signs and symptoms in all individuals, because these observations may be seen in patients with radicular, referred and/or local low back pain, they should be considered in the evaluation of the symptomatic patient presenting with a clinical lumbosacral syndrome.
Imaging recommendations, in addition to the usual close scrutiny of these posterior spinal elements and perispinal soft tissues on CT and MRI, include the acquisition of high-resolution multiplanar CT reconstructions, and fat-suppressed T2 weighted fast-spin- or turbo-spin-echo sequence MRI in at least one plane in every examination of the lumbar spine.
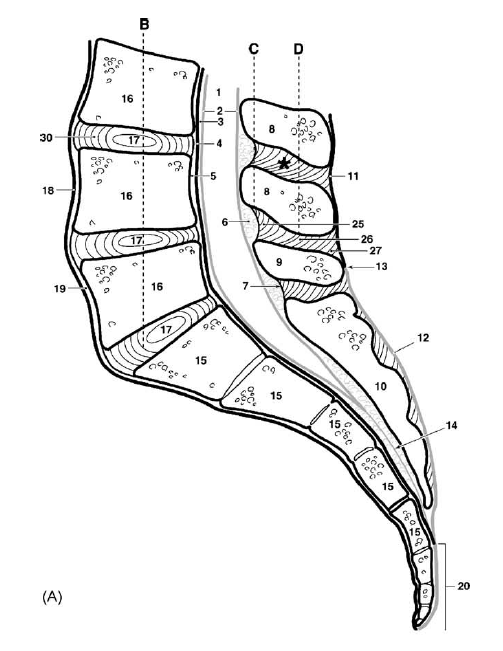
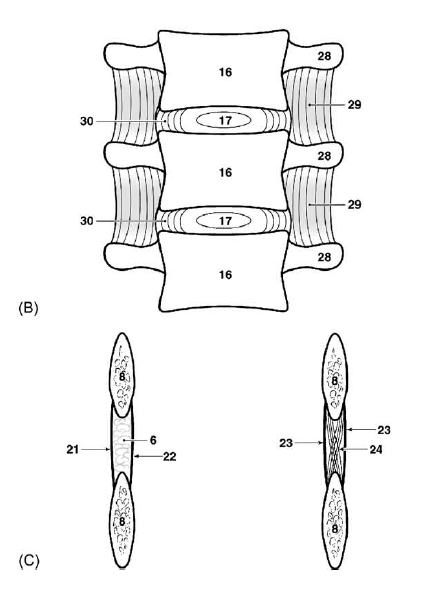
Normal and variant anatomy of the lumbosacral spine
Fig. 1. Normal osseous and ligamentous anatomy of the lumbosacral spine. (A) Midline sagittal section diagram of the lumbosacral spinal ligaments and related spaces. (B) Coronal section diagram through the mid-portions of the lower lumbar vertebrae and intervertebral disks with the anterior tissues removed. Note also the transverse processes and inter-transverse ligaments. (C) Coronal section diagram through anterior aspect of interspinous ligament and adjacent spinous processes. (D) Coronal section diagram through mid-aspect of interspinous ligament and adjacent spinous processes.
1, Spinal subarachnoid space; 2, thecal sac; 3, anterior epidural space; 4, posterior longitudinal ligament; 5, retrovertebral subligamentous space; 6, median retrothecal fat pad (posterior epidural space); 7, junction of halves of interspinous ligament with the ligamenta flava; 8, normal spinous processes of L3 and L4; 9, normally mildly hypo-plastic spinous process of L5; 10, midline sacral spinous tubercles; 11, supraspinous ligament; 12, erector spinae muscle tendons and deep fibers of the lumbosacral fascia; 13, variation in termination of supraspinous ligament (L3–L5); 14, filum terminale; 15, sacral spinal segments; 16, lumbar vertebral bodies; 17, nucleus pulposus of the lumbar intervertebral disk(s); 18, anterior longitudinal ligament; 19, prevertebral sub-ligamentous space; 20, coccyx; 21, right half of interspinous ligament anteriorly; 22, left half of interspinous ligament anteriorly; 23, combined right and
left halves of the interspinous ligament in its middle and posterior extent; 24, fibers of interspinous ligament shown crossing the midline; 25, anterior (ventral) segment of interspinous ligament originating in ligamenta flava on each side and terminating in inferior margin of the suprajacent spinous process; 26, middle segment of interspinous ligament originating in superior margin of subjacent spinous process and terminating in suprajacent spinal process; 27, posterior (dorsal) segment of interspinous segment originating in the superior margin of the subjacent spinous process and terminating in the supraspinous ligament (at levels where it exists) or the erector spine muscle tendons (below the level of the supraspinous ligament); 28, transverse recesses; 29, intertransverse ligaments and intertransversarii muscles; 30, annulus fibrosus of the intervertebral disk(s).
and the junction between the two (black arrow).
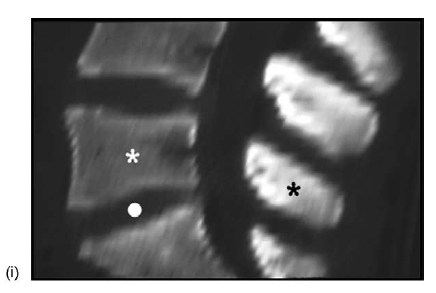
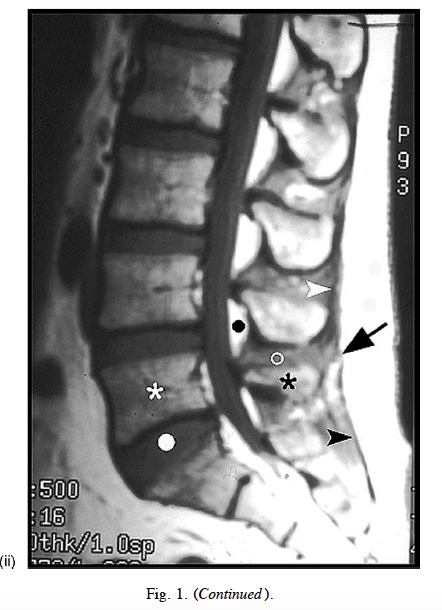
Note the posterocranial orientation of the fibers of the interspinous ligament (B–D). (E) Medical imaging studies: (i) midline sagittal CT reconstruction; normal posterior wedge configuration of the L5 vertebral body (white asterisk) and the L5-S1 intervertebral disk (white dot); normal hypoplasia of the L5 spinous process (black asterisk: compare with (A)). (ii) Midline T1-weighted MRI showing again the posterior wedge configuration of the L4 and L5 (white asterisk) vertebral bodies and the lower lumbar intervertebral disk(s) (white dot), and the hypoplastic L5 spinous process (black asterisk: compare with (A)).
Note the shape and intensity of the retrothecal fat pad(s) (black dot) and the interspinous ligament(s) (white circle). Also note the supraspinous ligament (white arrowhead), the midline inferior extension of the lumbosacral fascia (black arrowhead),
Pathologic anatomy of the lumbosacral spine related to or accompanying collapse of the intervertebral disc
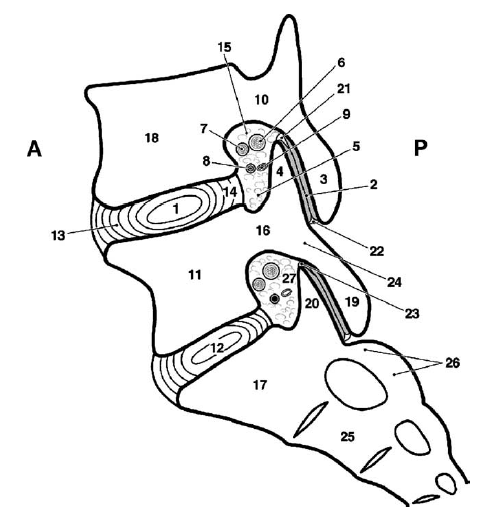
Fig. 2. Normal sagittal appearance of the L4-L5 and L5-S1 neural foramen. (A) Parasagittal section diagram of the spinal neural foramen.
1, L4-L5 intervertebral disk; 2, L4-L5 posterior facet (i.e., zygapophyseal) joint space and articular cartilage; 3, inferior articular facet process of L4; 4, superior articular facet process of L5; 5, inferior recess of the L4-L5 spinal neural foramen; 6, dorsal root ganglion of the L4 spinal nerve dorsal root; 7, ventral root; 8, radiculomedullary artery at L4-L5; 9, radiculomedullary vein at L4-L5; 10, L4 pedicle; 11, L5 vertebral body; 12, L5-S1 intervertebral disk; 13, anterior anular fibers of the L4-L5 intervertebral disk; 14, posterior anular fibers of the L4-L5 intervertebral disk; 15, superior recess of the L4-L5 spinal neural foramen; 16, L5 pedicle; 17, S1 vertebral segment; 18, L4 vertebral body; 19, inferior articular process of L5; 20, superior articular process of S1; 21, superior
articular recess of the L4-L5 posterior spinal facet joint; 22, inferior articular recess of the L4-L5 posterior spinal facet joint; 23, superior articular recess and meniscoid of the L5-S1 posterior spinal facet; 24, pars interarticularis of L5; 25, S2 vertebral segment; 26, intermediate sacral crest at S1-S2; 27, intraforaminal fat.
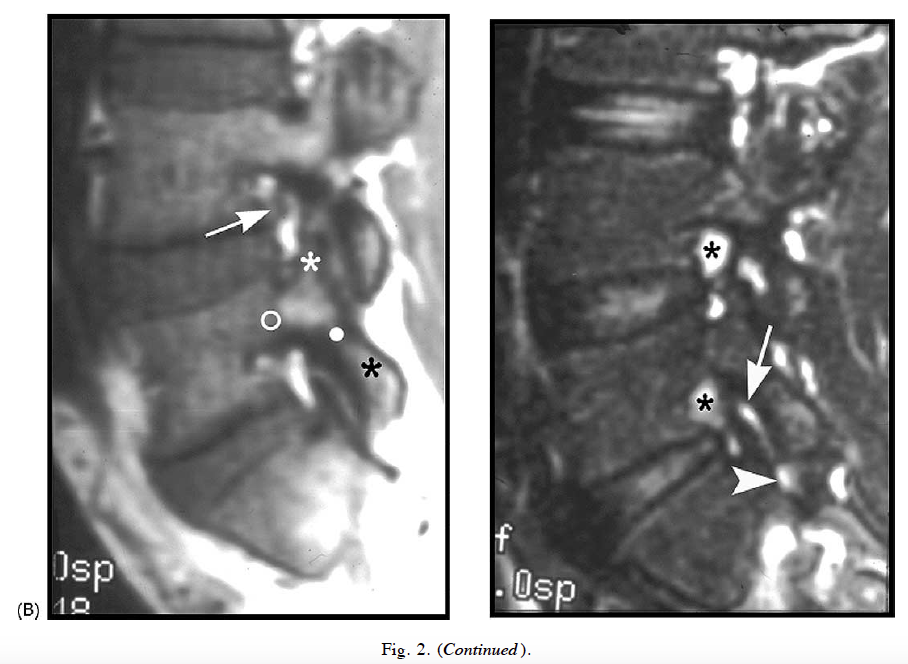
A: anterior, P: posterior. (B) Medical imaging studies: (i) lateral parasagittal CT reconstruction showing the bony structure defining the spinal neural foramen (compare with (A)). (ii) Lateral parasagittal T1-weighted MRI showing the pedicle (white circle) of L5, the superior articular process (white asterisk: zygapophysis) of L5, the inferior articular process (black asterisk: zygapophysis) of L5, the pars interarticularis (white dot) of L5; and a portion of the neurovascular bundle (arrow) exiting-entering the L4-L5 neural foramen. (iii) Lateral parasagittal T2-weighted fat-suppressed MRI showing normal fluid within the superior (arrow) and inferior (arrowhead) recesses of the
L5-S1 posterior spinal facet (zygapophyseal) joint on one side, and the normal high intensity of the dorsal root ganglia (black asterisks) within the neural foramina (compare with (A)).
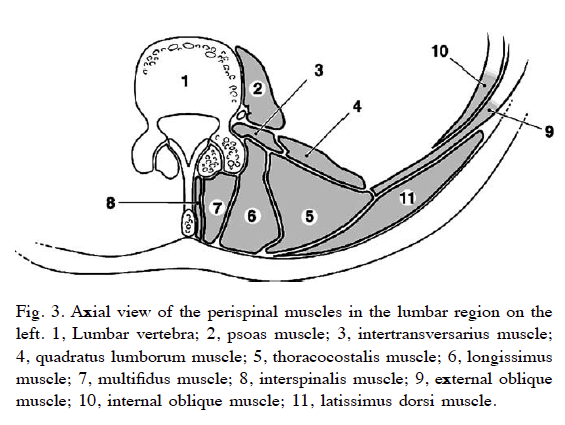
Fig. 3. Axial view of the perispinal muscles in the lumbar region on the left.
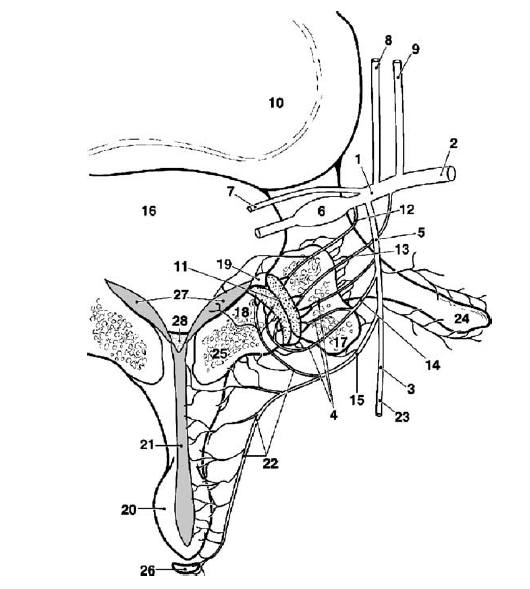
Fig. 4. Innervation of structures of dorsal (posterior) aspect of spinal column.
1, Main trunk of spinal nerve; 2, ventral ramus of spinal nerve; 3, lateral branch of dorsal ramus of spinal nerve; 4, neural fibers to posterior dorsal ramus of spinal nerve; 5, dorsal ramus of spinal nerve; 6, dorsal nerve root and ganglion; 7, ventral nerve root; 8, gray ramus communicans; 9, white ramus communicans; 10, intervertebral disk; 11, articular cartilage of posterior spinal facet (i.e., zygapophyseal) joint; 12, neural fibers from main trunk of spinal nerve; 13, neural fibers to posterior facet joint from ventral ramus of spinal nerve; 14, neural fibers to posterior facet joint from dorsal ramus; 15, medial branch of dorsal ramus of spinal nerve; 16, central spinal canal; 17, superior articular facet process; 18, inferior articular facet process; 19, zygapophyseal joint space
and capsule; 20, spinous process; 21, interspinous ligament; 22, medial neural branches ramifying within posterior facet joint, the lamina, spinous process, interspinous ligament, and supraspinous ligament; 23, branch of dorsal ramus ramifying within posterior perispinous tissues; 24, transverse process; 25, lamina; 26, supraspinous ligament; 27, ligamenta flava; 28, median retrothecal fat pad.
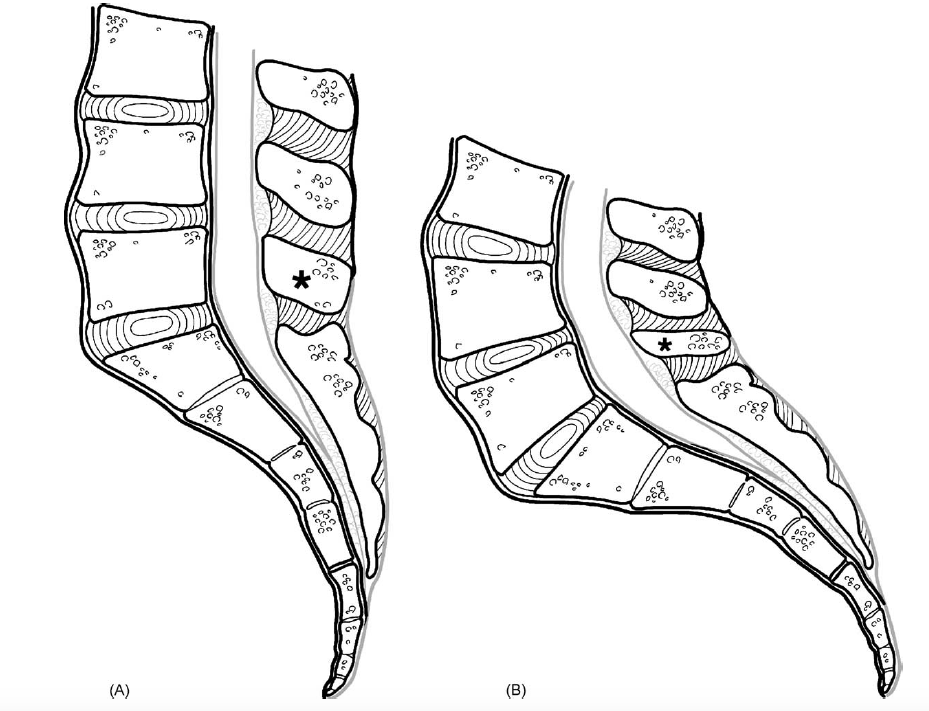
Fig. 5. Variant anatomy of the lumbosacral spine.
(A) Straight or hypolordotic spine. The spinal lordotic curvature in this example overall is minimal, or absent in extreme cases, in part because the lower lumbar vertebrae and intervertebral disks are less than normally wedge-shaped (i.e., rectangular shape in this example). Note the mildly hyperplastic L5 spinous process (asterisk). (B) Hyperlordotic (i.e., swayback) spine. The spinal lordotic curvature in this example is exaggerated and the sacrum tends to be more horizontal than normal. Note the hypoplastic L5 spinous process (asterisk) and the exaggerated wedge shape of the vertebral bodies and intervertebral disks. Compare with Fig. 1A. Also note the somewhat horizontally angled sacrum.
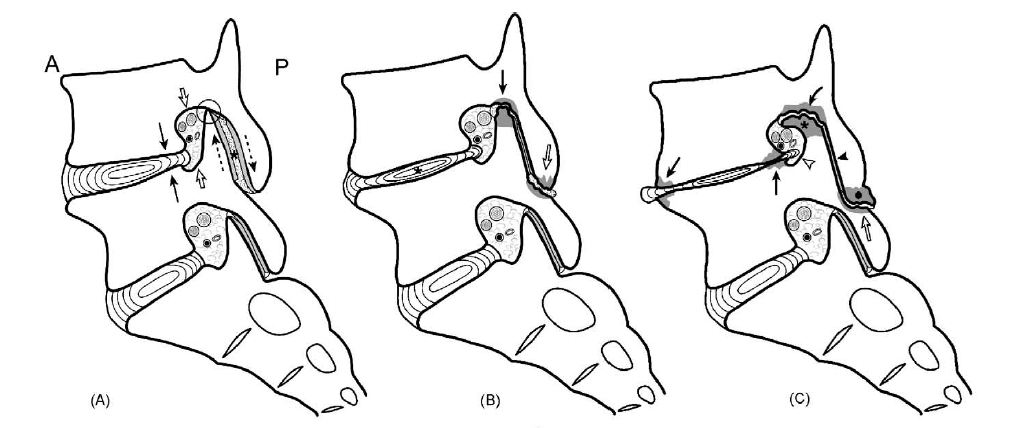
(A) Posterior or spinal facet joint subluxation associated with early intervertebral disk collapse. Note the mild L4-L5 intervertebral disk space narrowing (solid arrow), the superoinferior narrowing of the spinal neural foramen (open arrows), the superoinferior subluxation of the posterior spinal facet joint (dashed arrows), and the early collision and sclerosis of the apex of the superior articular process of L5 and the overlying pars interarticularis of L4 (circled area). This will result in many or all cases in posterior spinal facet joint(s) gapping (asterisk) and effusion (coarse stippling) at some time during this pathologic process.
(B) Collision and blunt erosion of the apices of the superior and inferior articular processes of the posterior spinal facet (i.e., zygapophyseal) joints and related bony spinal structures. With further narrowing of the intervertebral disk (asterisk), there may be blunting of the apex of the superior articular process and associated erosion of the anteroinferior aspect of the anteroinferior aspect of the overlying upper pars interarticularis of the suprajacent vertebra (solid arrow with shading). Note the early narrowing/erosion of the posterior spinal facet joint articular cartilage.
(C) Curved remodeling of superior articular facet process and neoarthrosis formation between the apex of the superior articular facet process and the suprajacent pars interarticularis. The superior articular process may eventually undergo a curved remodeling (asterisk), partially associated with osteophytic overgrowth. At the same time, a neoarthrosis (curved arrow) may form between the remodeled superior facet process and the overlaying bone of the undersurface of the suprajacent pedicle and pars interarticularis. Concomitantly a neoarthrosis (open arrow) may form between the apex of the inferior facet process (dot) and the posterior surface of the subjacent pars interarticularis. Anterior and posterior spinal facet joint articular cartilage has been eroded (solid arrowhead).
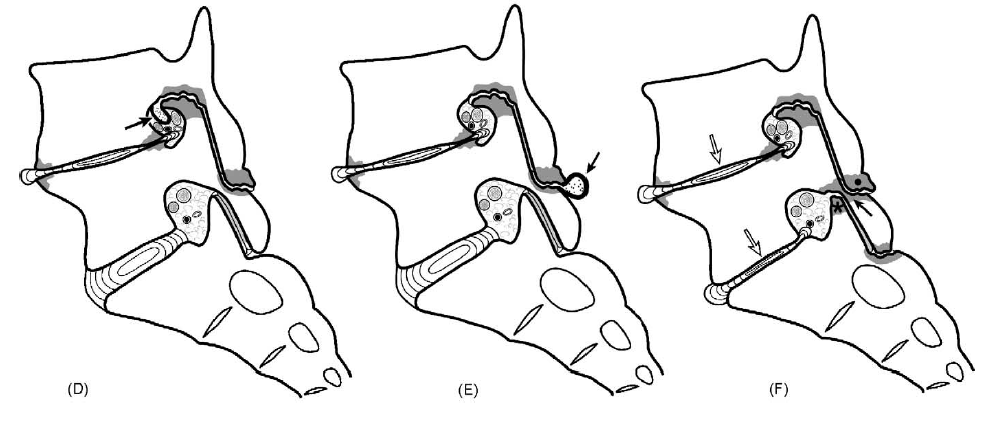
(D) Neocyst formation off of the neoarthrosis between the superior articular facet process and the superjacent pedicle-pars interarticularis. A neocyst (arrow: coarse stippling) that may communicate with the adjacent posterior spinal facet joint may form off of the neoarthrosis between the superior articular facet process and the inferior surface of the suprajacent pedicle-pars interarticularis. This neocyst may extend into the spinal neural foramen and central spinal canal, thereby narrowing these areas, and into the lateral/posterior perispinal soft tissues. Pathologically the cyst typically has a thick wall and a small central cavity. Histologically this cyst may not be lined by synovial tissue in which case it is a neocyst or pseudocyst, or may be lined by synovial tissue, thereby representing a true synovial cyst.
(E) Neocyst formation off of the apex of the inferior articular facet process and the subjacent pars interarticularis. A neocyst (arrow: coarse stippling) that may communicate with the adjacent posterior spinal facet joint may form off of the neoarthrosis between the apex of the inferior articular facet process and the posterior surface of the subjacent pars interarticularis. This neocyst will extend into the perispinous soft tissues. The neocyst characteristically has a thick wall and small cavity. As noted above, this cyst may be a neocyst of a true synovial cyst, a histologic distinction.
(F) Erosive pars interarticularis thinning: With collapse of the adjacent intervertebral disks at and suprajacent to the lumbosacral junction (open arrows), erosion of the intervening pars interarticularis (solid arrow) may occur anteriorly and posteriorly: the suprajacent inferior articular facet process (dot) erodes posteriorly and the subjacent superior articular facet process (asterisk) erodes anteriorly. This thins and structurally weakens the pars interarticularis.
(G) Degenerative insufficiency fracture of the pars interarticularis. With further erosion and continued stresses, an insufficiency fracture of the pars interarticularis may occur (dashed circle). This may then allow unrestricted degrees of acquired anterolisthesis to result (dashed arrow).
(H) Collisional articular facet process fracture. With continued stresses placed upon the remodeled and osteophytically overgrown posterior spinal articular facet processes, the superior (asterisk) or inferior (dot) articular facet process or attached brittle osteophytes may fracture (solid arrows: 1, 2). This may yet further narrow the spinal neural foramen at this level (open arrows).
(I) Articular process fracture fragment distraction/displacement. With continued somatic movements, the superior (asterisk) and inferior (dot) articular fracture fragments may go to nonunion and become distracted or displaced (curved arrows). The former further narrow the involved spinal neural foramen. The loss of this buttressing effect then allow further degenerative narrowing or absolute collapse of the intervertebral disk (open arrows), and consequently further narrowing (i.e., stenosis) of the spinal neural foramen at this level.
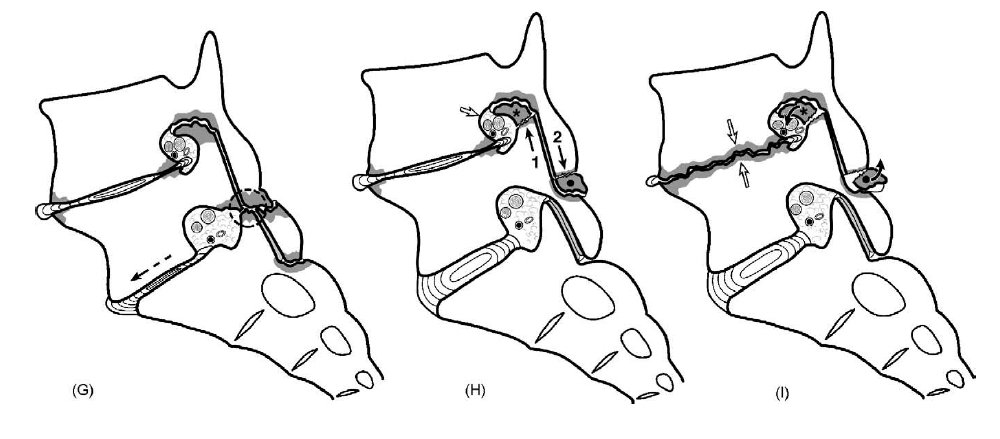
(J) Medical imaging studies:
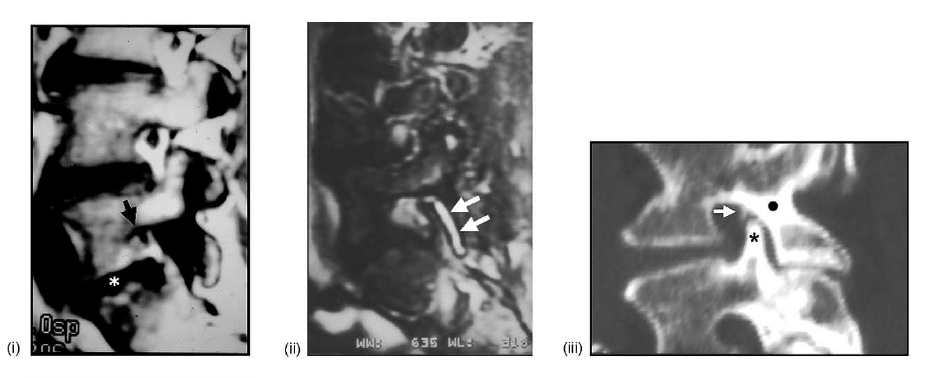
(i) parasagittal T1-weighted MRI showing collapse of the L5-S1 disk (asterisk) and superoinferior narrowing of the spinal neural foramen (arrow: compare with (A)).
(ii) Parasagittal T2-weighted fat-suppressed MRI showing the posterior spinal facet (zygapophyseal) joint effusion (arrows: compare with (A)).
(iii) Parasagittal CT reconstruction showing the collision of the superior facet process (asterisk) with the overlying pars interarticularis-pedicle junction (dot), and the minor associated osteophytosis (arrow).
(iv) Parasagittal CT reconstruction showing the bony excavation/erosion of the undersurface of the pars interarticularis at the L4 and L5 levels (arrows).
(v) Parasagittal CT reconstruction showing truncation of the tip of the superior articular facet process of S1 (arrow: compare with (B) and the sharp, pointed termination of the superior articular process at the L4-L5 level above: arrowhead).
(vi) Parasagittal T1-weighted MRI showing again the truncation of the tip of the articular facet process (asterisk) of S1 (compare with (B)).
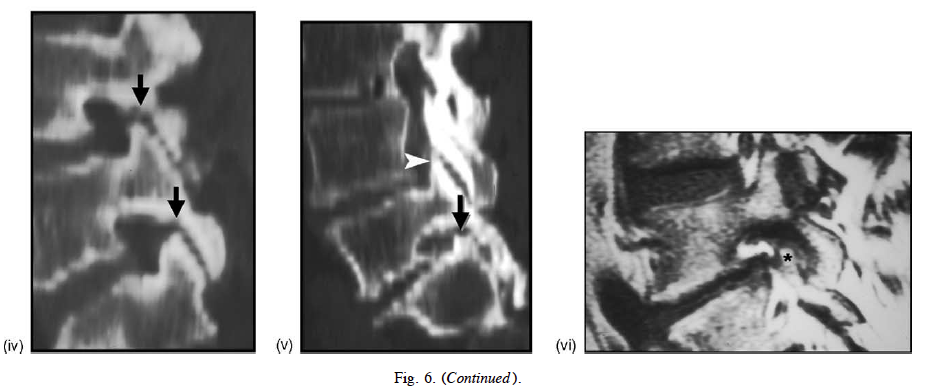
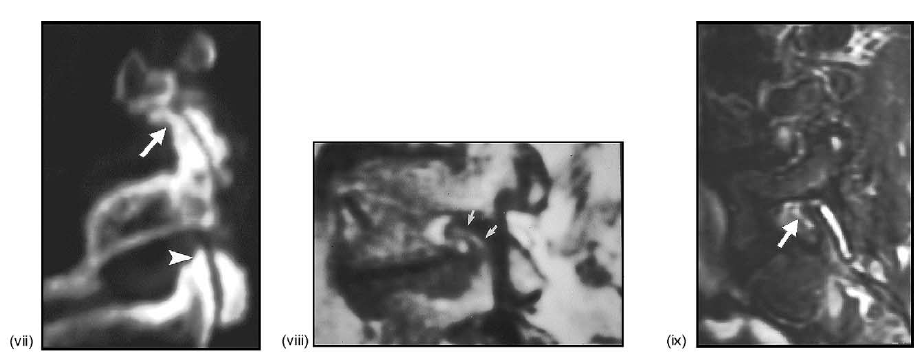
(vii) Parasagittal CT reconstruction showing curved remodeling of the superior articular facet process (arrow) of L4-L5 (compare
with (C) and the straight, pointed configuration of the level below: arrowhead).
(viii) Parasagittal T1-weighted MRI showing another case of curved remodeling of the superior articular facet process (arrows; compare with (C)).
(ix) Parasagittal T2-weighted, fat-suppressed MRI showing an anteriorly directed periarticular neocyst (arrow: i.e., synovial cyst) extending into the spinal neural foramen (compare with (D)).
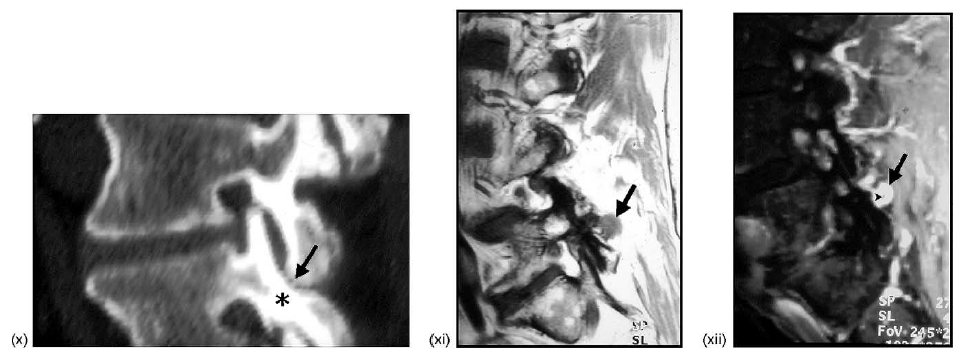
(x) Parasagittal CT reconstruction showing the collision of the tip of the inferior articular facet process of L4 (arrow) with the posterior–superior aspect of the subjacent pars articularis of L5 (asterisk) (compare with (B)).
(xi) Parasagittal T1-weighted MRI showing a posterior neocyst (arrow: i.e., synovial cyst) extending posteriorly from the inferior aspect of the zygapophyseal joint at L4-L5 (compare with (E)).
(xii) Parasagittal T1-weighted fat-suppressed, IV gadolinium-enhanced MRI showing enhancement of the thickened rim of the posterior neocyst (arrow); note the small non-enhancing central area of the cyst (arrowhead; compare with (E)).
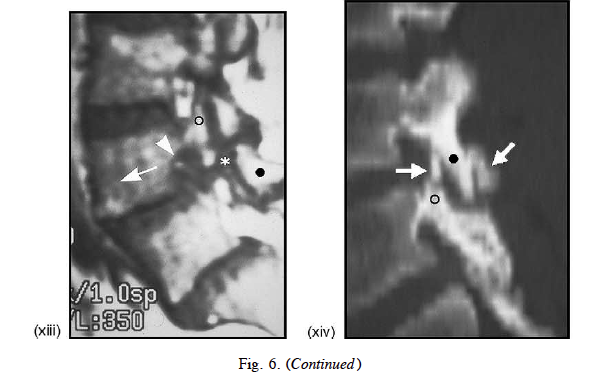
Fig. 6. Alterations in the posterior spinal facet (i.e., zygapophyseal) joints related to intervertebral disk collapse.
(xiii) Parasagittal T1-weighted MRI showing minor spondylolisthesis of L4 on L5 (arrow) secondary to acquired lysis of the pars interarticularis (asterisk) of L5; note the separation of the superior (circle) and inferior (dot) articular processes, the gap between the two (asterisk), and the complete obliteration (i.e., stenosis: arrowhead) of the superior recess of the L4-L5 neural foramen (compare with (G)). (xiv) Parasagittal CT reconstruction showing fatigue fractures of the inferior (arrow to reader’s right) and superior (arrow to reader’s left) articular facet processes of L3 (dot) and L4 (circle), respectively (compare with (I)).
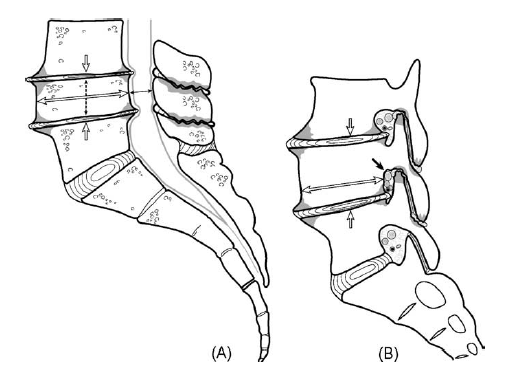
Fig. 7. Radial expansion remodeling of vertebral body.
(A) Radial expansion remodeling of the vertebral body between suprajacent and subjacent intervertebral disk collapse associated with central spine canal stenosis. The vertebral body between two adjacent collapsed intervertebral disks (open, single-headed arrows) may undergo radial expansion remodeling circumferentially in the horizontal plane (open, double-headed arrow). At the same time, there will be a superoinferior narrowing of the vertebral body (open, dashed double-headed arrow) producing a bony flat remodeling, or pancaking of the vertebra. This results in anteroposterior narrowing of the central spinal canal (solid double-headed arrow) and its lateral recesses.
(B) Radial expansion remodeling of the vertebral body associated with spinal neural foramen stenosis. The radially expanded vertebral body (open, double-headed arrow) between two collapsed intervertebral disks (open, single-headed arrows) results in anteroposterior narrowing of the spinal neural foramen (solid arrow) at this level. This stenosis alteration may be asymmetric, side-to-side.
(C) Medical imaging studies:
(i) midline sagittal T1-weighted MRI showing degeneration of the L3-L4 and L4-L5 intervertebral disks and associated flattening in the superoinferior dimension, and elongation in the anteroposterior dimension of the intervening L4 vertebral body (middle double-headed arrow); note the relative normal dimensions of the L1 and L5 vertebrae (upper and lower double-headed arrows, respectively) by comparison (compare with (A)).
(ii) Parasagittal T1-weighted MRI showing anteroposterior narrowing of the L4-L5 spinal neural foramen (arrow) as a consequence of the vertebral body elongation at the L4 level (compare with (B)); some superoinferior narrowing of the L4-L5 neural foramen is also present as a result of L4-L5 degenerative intervertebral disk collapse (asterisk).
Fig. 8. Degenerative alterations in the interspinous ligaments and interspinous space.
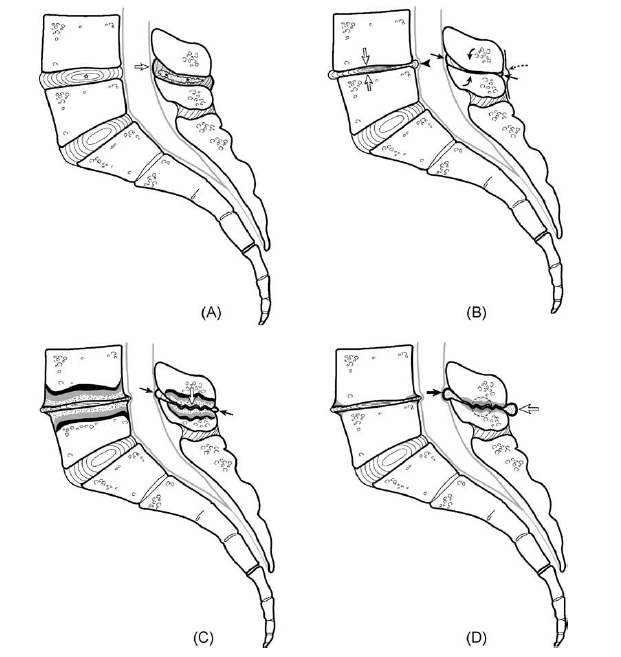
A, Interspinous ligament sprain with or without intervertebral disk degeneration and associated spinal instability with segmental motion-related stresses. Acute, subacute and chronic motion-related stresses may lead to a type of degenerative ligamentous sprain (i.e., edema, ligamentous fiber tears, frank rupture/avulsion) of the interspinous ligament (asterisk/shading). Interspinous ligament redundancy will bulge posteriorly and anteriorly; the latter will replace/displace varying degrees of the segmental retrothecal fat pad(s) (open arrow). These interspinous ligament sprains may be hyperintense on T1- and T2-weighted imaging sequences, presumably as a result of high
protein content. Ligamentous degenerative change may occur before, simultaneously with, or following intervertebral disk degeneration (asterisk).
(B) Spinous process collision associated with progressive interspinous degenerative alteration (i.e., Baastrup’s phenomenon). With progressive intervertebral disk collapse (open arrows), there may be a bony collision of the spinous processes of the adjacent vertebrae (solid curved arrows) at and suprajacent to the lumbosacral junction. Interspinous ligament redundancy (solid straight arrows) together with bulging of the posterior aspect of the intervertebral disk (arrowhead) into the central spinal canal will produce some degree of central spinal canal stenosis. Note that the redundant supraspinous ligament (dashed arrow) will bulge into the perispinous soft tissues (dashed curved arrow).
(C) Interspinous neoarthrosis associated with intervertebral disk collapse; associated stress-related marrow alterations within the spinous process marrow and vertebral bodies. With further collapse of the intervertebral disk and increased segmental instability/motion, a neoarthroses (i.e., pseudoarthrosis) may develop between the spinous processes of adjacent vertebral levels (open arrow). The thickened interspinous ligament will protrude peripherally/radially in the axial plane (solid arrows). These phenomena will be predisposed to in individuals with spinous processes that are larger in the superoinferior dimension and in individuals with marked lumbosacral lordosis (i.e., hyperlordosis: “sway back”). Spinous process and vertebral body marrow edema (coarse stippling: type 1 marrow alteration), fatty marrow infiltration (gray shading: type II marrow alteration) and/or bony sclerosis (black shading: type III marrow alteration) may result from these ongoing intervertebral interspinous stresses.
(D) Neocyst (i.e., pseudocyst) formation extending from an interspinous neoarthrosis. Continued stresses exerted upon the interspinous ligament and adjacent spinous processes may eventually result in neocyst formation extending off of the interspinous neoarthrosis. These neocysts may be multiple and may extend posteriorly (open arrow), laterally (dashed circle), or anteriorly (solid arrow). The latter may significantly contribute to stenosis of the central spinal canal.
(E) Medical imaging studies:
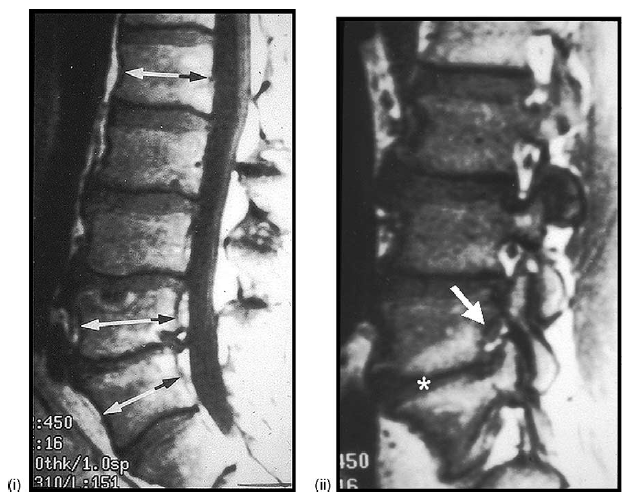
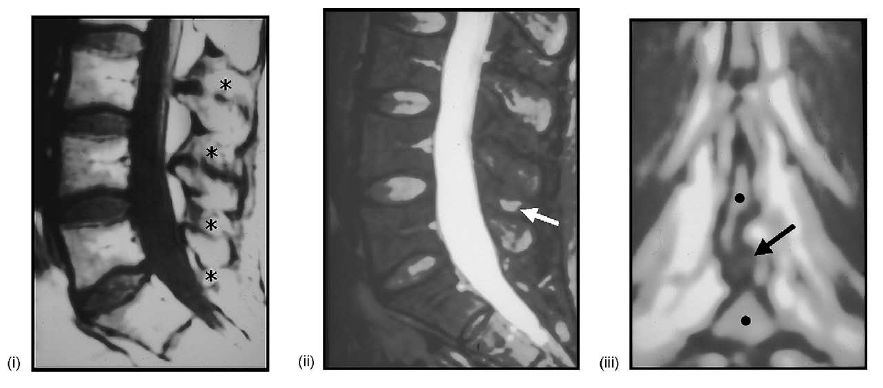
(i) midline sagittal T1-weighted MRI showing hyperintensity of the interspinous ligaments at multiple levels (asterisks). (ii) Midline sagittal T2-weighted, fat-suppressed MRI showing isolated hyperintensity of the L5-S1 interspinous space (arrow) indicating degeneration and possible cystic alteration of the interspinous ligament (compare with (A)). (iii) Coronal T1-weighted MRI showing the rounded appearance of the interspinous ligament (arrow), between the spinous processes of L5-S1 (dots).
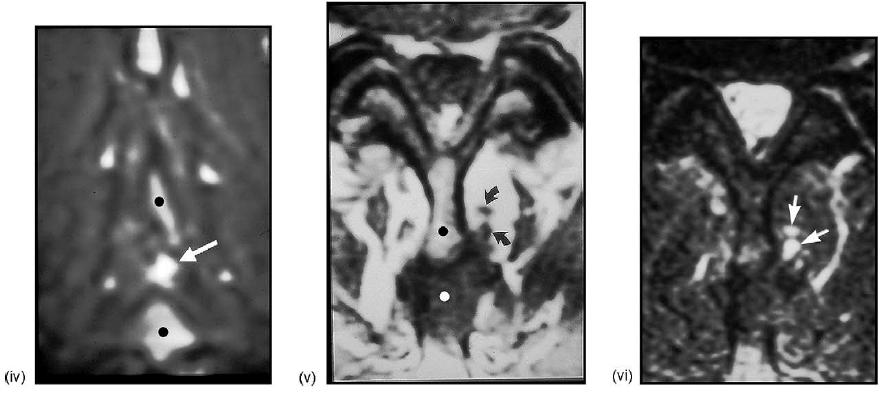
(iv) Coronal T2-weighted, fat-suppressed MRI showing again the apparent cystic degeneration of the interspinous ligament situated between the spinous processes of L4 and L5 (dots; compare with iv). (v) Axial T1-weighted MRI showing multiple rounded paraspinous soft tissue structures (arrows); also note the spinous process of L5 (black dot) and the redundant-hypertrophic inter-supraspinous ligament(s) (white dot) (compare with (D)). (vi) Axial T2-weighted, fat-suppressed MRI showing the hyperintense nature of the paraspinous cysts (arrows; same patient in (E) v–vi).
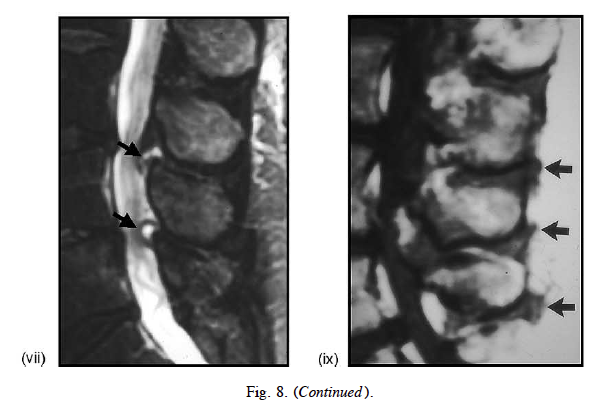
(vii) Sagittal T2-weighted, fat-suppressed MRI showing two interspinous cysts extending into the posterior aspect of the central spinal canal at L3-L4 and L4-L5 (arrows; compare with (D)). (viii) Midline sagittal T1-weighted MRI showing multilevel posterior redundancy-hypertrophy of the supraspinous ligament (arrows; compare with (B)).
Fig. 9. Degenerative retrolisthesis associated with intervertebral disk collapse and degeneration of related spinal structures.
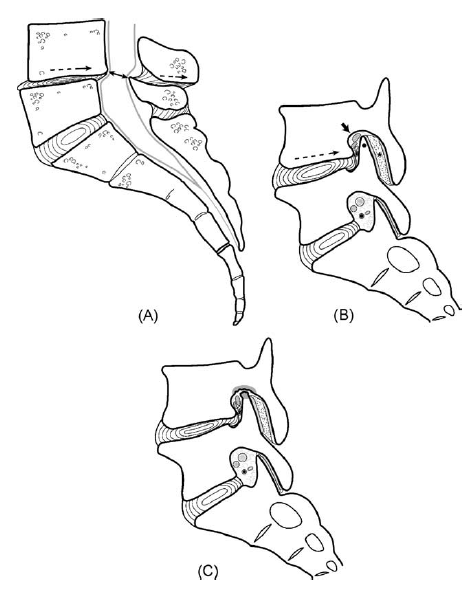
(A) Degenerative retrolisthesis with central spinal canal stenosis. With intervertebral disk collapse and degeneration of related spinal structures (e.g., intraspinal ligaments, degenerative retrolisthesis may occur (dashed arrows). This results in stenosis of the central spinal canal (double-headed arrow).
(B) Anteroposterior posterior spinal facet (i.e., zygapophyseal) joint dislocation. With the retrolisthesis of the suprajacent vertebral body (dashed arrow), there will be an anteroposterior posterior spinal facet joint dislocation (asterisk) associated with a joint effusion (coarse stippling). This will narrow the anteroposterior diameter of the spinal neural foramen (solid arrow). In addition, the apex of the superior articular facet process (dot) may protrude directly into the superior recess of the spinal neural foramen.
(C) Erosion of the apex of the superior articular facet process and pedicle. With further disk collapse there maybe an excavative erosion
of the apex of the superior articular facet process and suprajacent pedicle (shading).
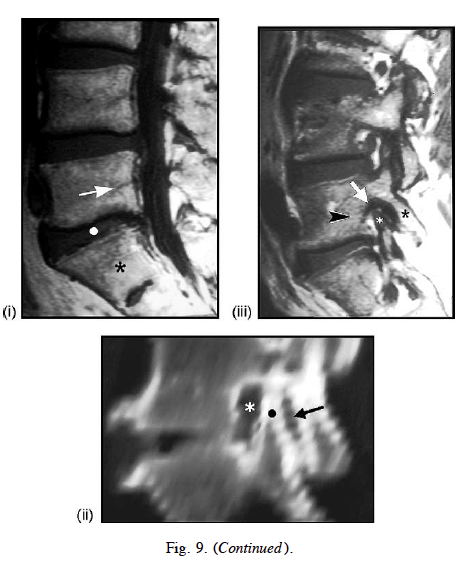
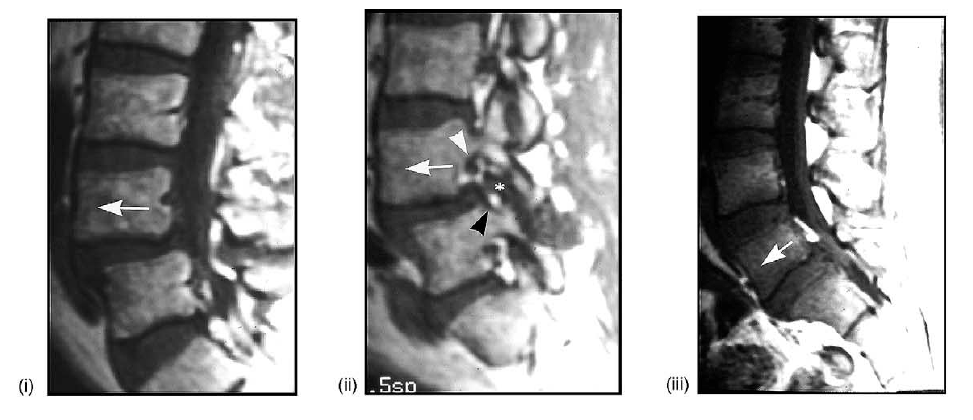
(D) Medical imaging studies: (i) midline sagittal T1-weighted MRI showing partial disk collapse at L5-S1 (dot) associated with very
minor degenerative retrolisthesis of L5 (arrow) on S1 (asterisk; compare with (A)). (ii) Parasagittal CT reconstruction showing anteroposterior posterior spinal facet joint space “gapping” (arrow) resulting from relative anterior displacement of the superior facet process of S1 (dot) into the spinal neural foramen causing anteroposterior narrowing of the foramen (asterisk; compare with (B)). (iii) Parasagittal T1-weighted MRI showing minor retrolisthesis of L5 (arrowhead) on S1, with anterior displacement of the superior articular facet process (white asterisk) of S1 into the superior recess of the spinal neural foramen resulting in foraminal stenosis (arrow); there is relative consonant posterior displacement of the inferior articular process of L5 (black asterisk) compare with (B)).
Fig. 10. Degenerative anterolisthesis related to intervertebral disk collapse and degeneration of related spinal structure.
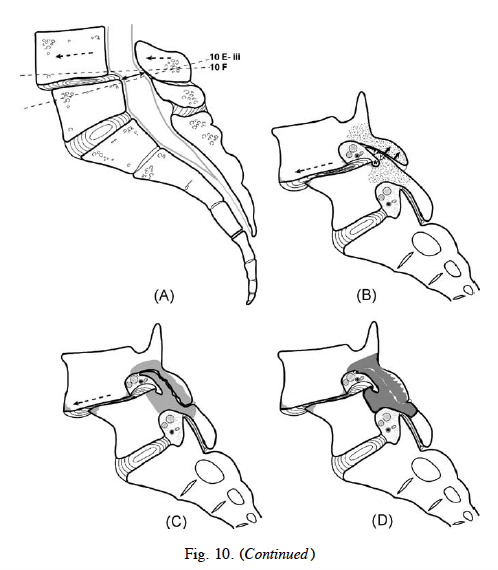
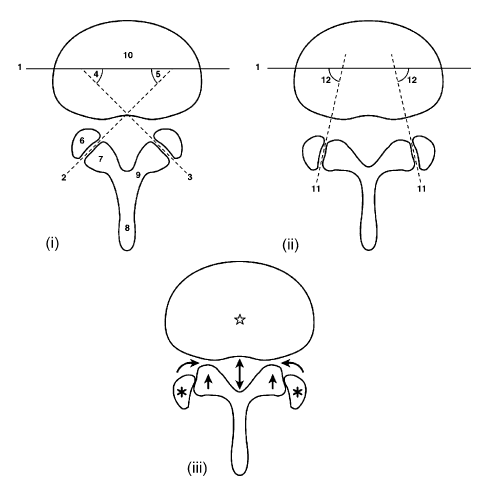
(A) Degenerative anterolisthesis. With collapse of the intervertebral disk and degeneration of related spinal structure (e.g., intraspinal ligaments), degenerative anterolisthesis (dashed arrows) of the suprajacent vertebral body may occur. This results in stenosis of the central spinal canal (double-headed arrow) (dashed lines: levels of sections in iii and F).
(B) Angular remodeling of the articular facet processes and Type I stress-related marrow alteration. In order for degenerative
anterolisthesis (dashed arrow) to occur, segmented anterior angular remodeling (i.e., bending) of the superior articular facet process (open arrows) of the subjacent vertebra and posterior angular remodeling of the inferior articular facet process (solid arrows) of the suprajacent vertebra must occur. Degenerative narrowing of the posterior articular facet joint space also takes place, initially occurring as a result of articular cartilage loss. During the active-progressive phase of this process, marrow edema (coarse stippling: type I marrow alteration) may be present within the affected segmental posterior articular facet processes, pars interarticularis (i) and connected pedicle(s). Radial anterior; posterior and lateral (not shown) paradiskal osteophytes (shaded areas) may be present. Note the narrowing of the inferior recess (asterisk) of the spinal neural foramen that results from anterior angular remodeling of the superior articular process.
(C) Type II stress-related posterior articular process/pars interarticularis pedicle marrow alterations. With continued anterior translational (i.e., shear: dashed arrow) stresses on the spine, fatty marrow infiltration (gray shading: type II marrow alteration) may result. Note the erosive changes of the respective posterior spinal fact joint articular processes.
(D) Type III stress-related posterior articular process/pars interarticularis/pedicle marrow alteration. Bony sclerosis (black shading: type III marrow alteration) of the pars interarticularis (i) articular facet process(es) and pedicle(s) of the involved vertebrae may eventually result.
(E) Sagittal with primary orientation (i.e., developmental), or secondary stress-related degenerative remodeling reorientation (i.e., acquired), of the posterior spinal facet (i.e., zygapophyseal) joint in the axial plane, consequent degenerative anterolisthesis.
(i) Normal posterior spinal facet joint angulation in the axial (transverse) plane. (ii) Increased sagittal plane orientation of the posterior spinal facet joint angulation in the axial plane. This sagittal plane orientation may be primary (i.e., developmental sagittal orientation) or acquired (i.e., degenerative remodeling).
(iii) Axial plane relationship of anterolisthetic suprajacent vertebra and its superior articular facet process (solid arrows) compared with the subjacent vertebral body (star) and its inferior articular facet processes (asterisks) in cases of sagittal facet joint angle orientation. Sagittal primary orientation of acquired reorientation of the posterior spinal facet joints in the axial plane results in anterolisthesis. This in turn causes stenosis of the central spinal canal (double-headed arrow), and simultaneous narrowing of the inferior recesses of the spinal neural foramina and lateral recesses of the central spinal canal (curved arrows).
1, Coronal plane of vertebral body; 2, posterior spinal facet (i.e., zygapophyseal) joint angle on the right side in the axial plane;
3, posterior spinal facet joint angle on the left side in the axial plane; 4, posterior spinal facet joint angulation on the left side with reference to the coronal plane of the spine; 5, posterior spinal facet joint angulation on the right side with reference to the coronal plane of the spine; 6, superior articular process of subjacent vertebra; 7, inferior articular process and contiguous pars interarticularis of suprajacent vertebra; 8, spinous process; 9, lamina; 10, vertebral body; 11, bilateral sagittal orientation of the posterior spinal facet joint angles; 12, relative enlargement of posterior spinal facet joint angles. Compare with E-i; 13, bilateral coronal orientation of the posterior spinal facet joint angles; 14, relative narrowing of posterior spinal facet joint angles. Compare with E-i and E-ii.
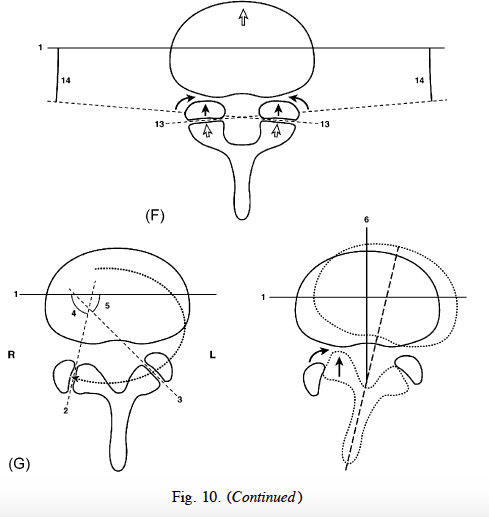
(F) Axial plane relationship of suprajacent anterolisthesis vertebral body and its inferior articular facet processes (open arrows) to subjacent superior articular processes in example of coronally oriented facet joint angulation in the axial plane. In the absence of a primary or acquired sagittal orientation of the posterior spinal facet joint angulations, the shear forces obtained at this level of the spine may still result in anterior angular remodeling of the superior articular processes (solid arrows) of the subjacent vertebra (not shown) and consequent stenosis of the inferior recess of the spinal neural foramina (see Fig. B) and the lateral recesses of the central spinal canal (curved arrows). (G) Segmental sagittal plane tropism (i.e., asymmetry of the posterior spinal facet (i.e., zygapophyseal) joints with consequent degenerative rotolisthesis (i.e., segmental rotoscoliosis).
(i) Tropism or posterior spinal facet joint asymmetry not infrequently is present before the onset of degenerative disease. Note the more sagittal orientation of the facet joint in this example on the right side, with reference to the axial plane. (Curved, dotted arrow: rotational stresses obtaining in right-foot dominant individual. Note the forces terminate at right angles to the posterior spinal facet joint angulation in the axial plane. Prior to segmental spinal degeneration alterations, this may be a biomechanically advantageous spatial orientation). (ii) Rotational segmental rotolisthesis (i.e., segmental rotoscoliosis) may accompany segmental spinal degenerative changes in cases of posterior spinal facet joint tropism. Note the segmental rotolisthesis that may occur in cases of pre-existing (i.e., developmental) posterior facet joint tropism. The suprajacent vertebral (dotted outline) rotates with reference to the subjacent vertebra (solid outline). This has the effect of unilateral anterior displacement of the posterior vertebral elements (straight arrow) and ipsilateral stenosis of the lateral recess of the central spinal canal and the inferior recess of the spinal neural foramen (curved arrow), on this side (dashed line: rotationally
shifted median sagittal plane of suprajacent vertebra). 1, Coronal plane of vertebral body; 2, posterior spinal facet joint relative sagittal angulation on the right side in the axial plane; (3) posterior spinal facet joint on the left side in the axial plane; (4) posterior spinal facet joint angulation with reference to
the coronal plane of the spine; (5) posterior spinal facet joint angulation on the right side with reference to the coronal plane of the spine; (6) median
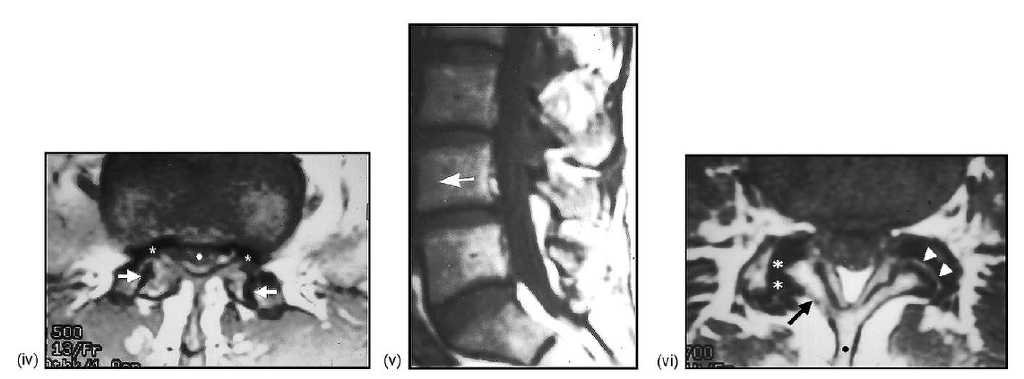
sagittal plane of subjacent vertebra. (H) Medical imaging studies: (i) midline sagittal T1-weighted MRI showing a grade I anterolisthesis of L4 on L5
(arrow: compare with (A)). (ii) Parasagittal T1-weighted MRI showing the anterolisthesis of L4 (arrow) on L5, the anterior angular bending/remodeling
of the superior articular process of L4 (asterisk), and the stenosis of the inferior recess (black arrowhead) and relative patency of the superior recess
(white arrowhead) of the L4-L5 spinal neural foramen; same case as in (i) (compare with (B)). (iii) Midline sagittal T1-weighted MRI showing grade
I anterolisthesis of L5 (arrow) on S1. (iv) Axial T1-weighted MRI at L5-S1 showing the near sagittal orientation of the angulation of the posterior
spinal facet joints (arrows) in the axial plane on both sides; note the stenosis of the central spinal canal (dot) and the spinal neural foramina bilaterally
(asterisks) (same case as in H,iii; compare with (E)). (v) Midline sagittal T1-weighted MRI in a different patient showing the very minor anterolisthesis
of L4 on L5 (arrow). (vi) Axial T1-weighted MRI showing a clockwise rotoscoliosis of L4 on L5, oblique orientation of the facet joint angulation in
the axial plane on the left side (arrowheads), and partial sagittal orientation of the posterior facet joint angulation on the right side (asterisks); note
the associated anterior displacement of the lamina and inferior articular facet process (arrow) on the right as compared to the patient’s left side, and
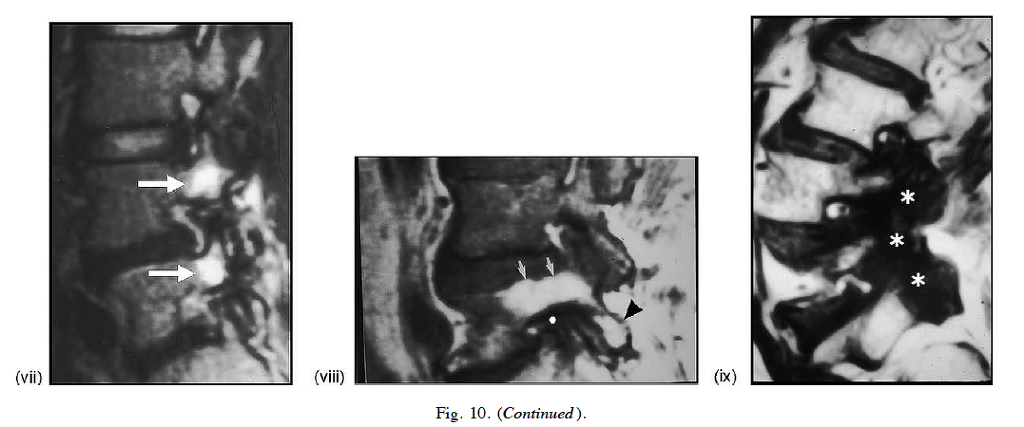
the displacement of the spinous process (dot) toward the right side as a result of the rotoscoliosis (compare with (G)). (vii) Parasagittal T2-weighted,
fat-suppressed MRI showing Type I hyperintense edematous vertebral marrow alterations involving the pedicles, pars interarticulari, and articular facet
processes at the L4 and L5 levels (arrows; compare with (B)). (viii) Parasagittal T1-weighted MRI showing Type II hyperintense fatty marrow alteration
within the pedicle (arrows) and inferior articular facet process (arrowhead) of L5; note the complete obliteration (i.e., stenosis) of the neural foramen at
L4-L5 (dot) (compare with (C)). (ix) Parasagittal T1-weighted MRI showing the Type III hypointense sclerotic alteration of the vertebral marrow within
the posterior bony structures at multiple spinal levels inferiorly (asterisks; compare with (D)).