Re:Depression과 관련된 영양 - 설탕금지, 오메가 3오일, 비타민 B3, 6, 9, 12, C, SAMe, 아연, 구리, 마그네슘,
작성자문형철작성시간19.08.27조회수492 목록 댓글 1beyond reason
미량원소 치유의학의 세계
영양물질과 관련된 우울증
미량원소로 치료하는 우울증
아연, 구리, 마그네슘, 비타민 C, 비타민 B 3, 6, 9, 12는 세로토닌, 도파민 합성과 관여
클릭클릭
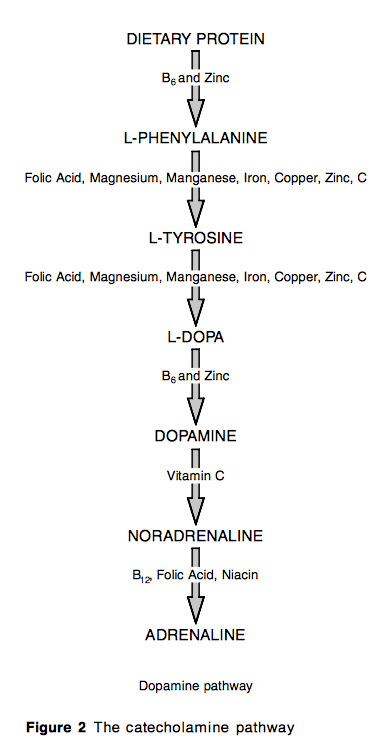
There is little doubt that the incidence of depression in Britain is increasing. According to research at the Universities of London and Warwick, the incidence of depression among young people has doubled in the past 12 years. However, whether young or old, the question is why and what can be done? There are those who argue that the increasingly common phenomenon of depression is primarily psychological, and best dealt with by counselling. There are others who consider depression as a biochemical phenomenon, best dealt with by antidepressant medication. However, there is a third aspect to the onset and treatment of depression that is given little heed: nutrition.
- 청소년 우울증이 증가추세에 있음. 12년사이에 두배 증가.
- 우울증은 생화학적 현상, 항우울제 연구는 많음.
- 그런데 영양적 관점의 탐구는 부족함.
Why would nutrition have anything to do with depression?
Firstly, we have seen a signicant decline in fruit and vegetable intake (rich in folic acid), in fish intake (rich in essential fats) and an increase in sugar consumption, from 2 lb a year in the 1940s to 150 lb a year in many of today’s teenagers. Each of these nutrients is strongly linked to depression and could, theoretically, contribute to increasing rates of depression.
- 엽산이 풍부한 음식섭취(과일, 야채) 부족, 오메가 3오일이 풍부한 생선섭취 부족, 설탕섭취 증가가 요즘 청소년들의 우울증가 증가와 명백한 관련이 있음.
Secondly, if depression is a biochemical imbalance it makes sense to explore how the brain normalises its own biochemistry, using nutrients as the precursors for key neurotransmitters such as serotonin.
- 우울증의 생화학적 불균형의 문제는 세로토닌과 연관성이 있음.
Thirdly, if 21st century living is extra-stressful, it would be logical to assume that increasing psychological demands would also increase nutritional requirements since the brain is structurally and functionally completely dependent on nutrients.
- 21세기는 과도한 스트레스 시대이고 미량원소와 미네랄 등의 영양소 요구량이 증가하는데 이와 우울증은 연관성이 있음.
So, what evidence is there to support suboptimal nutrition as a potential contributor to depression? These are the common imbalances connected to nutrition that are known to worsen your mood and motivation:
-
. blood sugar imbalances (often associated with excessive sugar and stimulant intake)
-
. lack of amino acids (tryptophan and tyrosine are precursors of serotonin and noradrenaline)
-
. lack of B vitamins (vitamin B6, folate, B12)
-
. lack of essential fats (omega-3).
우울증과 관련된 영양소
1) 설탕불균형 - 인슐린저항성
2) 아미노산(트립토판, 타이로신 - 세로토닌과 아드레날린 전구물질)
3) 비타민 B6, 9, 12 부족
4) 오메가 3 오일 부족
The sugar blues
One factor that often underlies depression is poor control of blood glucose levels. The symptoms of impaired blood sugar control are many, and include fatigue, irritability, dizziness, insomnia, excessive sweating (especially at night), poor concentration and forget- fulness, excessive thirst, depression and crying spells, digestive disturbances and blurred vision. These symptoms often precede measurable abnormalities in blood glucose, manifesting first as a decreased sensitivity to insulin, known as insulin resistance. One of the world’s experts on blood sugar problems, Professor Gerald Reaven from Stanford University in California, USA, estimates that 25% of normal, non-obese people have `insulin resistance’. Since the brain depends on an even supply of glucose it is no surprise to find that sugar has been implicated in aggressive behaviour,1 ± 6 anxiety,7 ,8 hyperactivity and attention deficit,9 de- pression,10 eating disorders,11 fatigue,10 and learning difficulties.1 2 ± 1 5
The second reason excessive consumption of refined sugar is undesirable is that it uses up the body’s vitamins and minerals and provides next to none. Every teaspoon of sugar uses up B vitamins for its catabolism, thereby increasing demand. B vitamins, as we will see, are vital for maintaining mood. About 98% of the chromium present in sugarcane is lost in turning it into sugar. This mineral is vital for keeping the blood sugar level stable.
The amino acid connection
There are often two sides to depression feeling miserable, and feeling apathetic and unmotivated. The most prevalent biochemical theory for the cause of these imbalances is a brain imbalance in two families of neurotransmitters. These are:
-
. serotonin, thought to primarily influence mood
-
. dopamine, noradrenaline, and adrenaline, thought to primarily influence motivation.
To test the theory that serotonin primarily controls mood, and adrenaline and noradrenaline control motivation, Antonella Dubini, from the Pharmacia and Upjohn Medical Department in Milan, Italy, gave 203 people suffering from low mood and motivation either a SSRI (selective serotonin reuptake inhibitor) drug, promoting serotonin, or a NARI (noradrenaline reuptake inhibitor) drug, promoting noradrenaline. Sure enough, the former was more effective at improving mood, while the latter was more effective at improving motivation.16
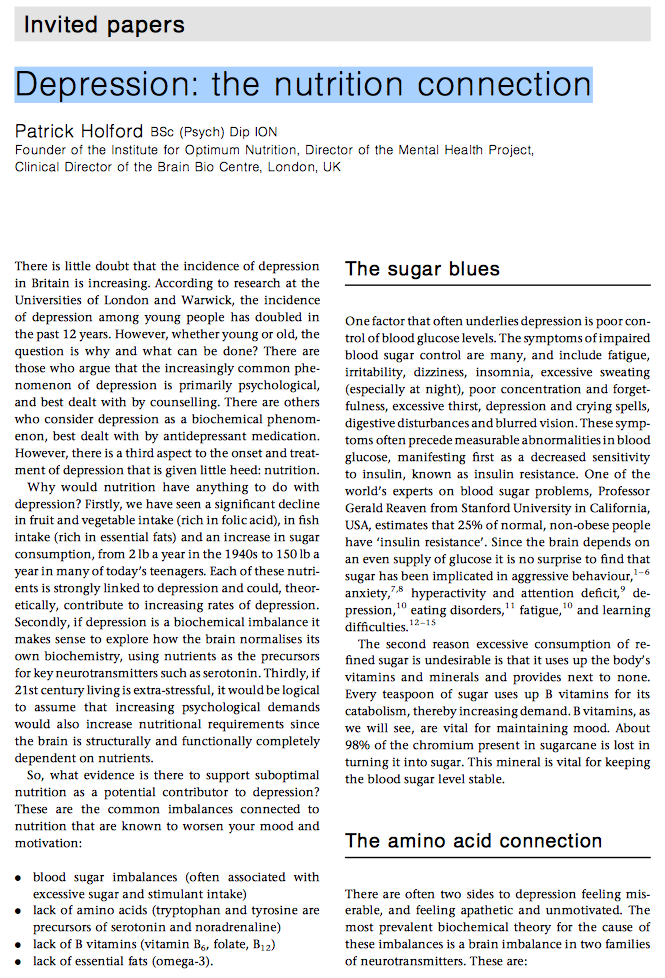
Figure 1 shows those nutrients that are required for the production of serotonin, dopamine, adrenaline and noradrenaline.
Depression and tryptophan
SSRI antidepressants are thought to work by stopping the reuptake of serotonin, thereby enhancing seroto- nin action within the synapse. The trouble is that these kinds of drugs induce unpleasant side effects in as many as a quarter of those who take them, and severe reactions in a minority. An alternative strategy would be to enhance the synthesis of serotonin by providing optimal amounts of precursor nutrients. But, does it work?
Serotonin is made from the amino acid tryptophan, a constituent of protein. Dr Philip Cowen and colleagues from the University of Oxford, UK, psy- chiatry department, wondered what would happen if you deprived people of tryptophan. They gave 15 vol- unteers who had a history of depression, but were currently not depressed, a nutritionally balanced drink that excluded tryptophan. Within seven hours 10 out of 15 noticed a worsening of their mood and started to show signs of depression. On being given the same drink, but this time with tryptophan added, their mood improved.1 7 Supplementing the amino acid tryptophan is already proven to improve mood. Don- ald Ecclestone, professor of medicine at the Royal Victoria In®rmary, Newcastle, UK reviewed the avail- able studies and concluded that supplementing tryp- tophan is an effective antidepressant, equivalent to tricyclic antidepressants.18
While supplementing tryptophan itself has proven a somewhat effective antidepressant, even more effec- tive is a derivative of tryptophan that is one step closer to serotonin. This is called 5-hydroxytryptophan, or 5-HTP for short. The ®rst study proving the mood- boosting power of 5-HTP was done in the 1970s in Japan, under the direction of Professor Isamu Sano of the Osaka University Medical School.19 He gave 107 patients 50 to 300 mg of 5-HTP per day, and within two weeks, more than half experienced improve- ments in their symptoms. By the end of the fourth week of the study, nearly three-quarters of the patients reported either complete relief or signi®cant improvement, with no side effects. This study was repeated by Nakajima et al. who also found that 69% of patients improved their mood.2 0 A trial in Germany found 5-HTP to be as effective as the tricyclic anti- depressant imipramine, with a fraction of the side effects.21 One double-blind trial headed by Dr Poldin- ger at the Basel University of Psychiatry, Switzerland gave 34 depressed volunteers either the SSRI anti- depressant ̄uvoxamine, or 300mg of 5-HTP. Each patient was assessed for their degree of depression using the widely accepted Hamilton Rating Scale, plus their own subjective self-assessment. At the end of the six weeks, both groups of patients had had a signi®cant improvement in their depression. However, those taking 5-HTP had a slightly greater improvement in each of the four criteria assessed ± depression, anxiety, insomnia and physical symptoms, as well as the patient’s self-assessment.22 Given that 5-HTP is less expensive and has signi®cantly fewer side effects, it is surprising that doctors and psychiatrists virtually never prescribe it.19,20,23 ±25
The recommended dosage of this amino acid, avail- able in any health food shop, is 100 mg of 5-HTP, two or three times a day, for depression. Some supple- ments also provide various vitamins and minerals such as B12 and folic acid, which may be even more effective because these nutrients help to turn 5-HTP into serotonin.
Depression in women
Women are three times as prone to low moods as men. Many theories as to why this is have been proposed, some psychological, some social, but the truth is that women and men are biochemically very different. The research of Mirko Diksic and colleagues at McGill University in Montreal, Canada demon- strates this. They developed a technique using positron emission tomography (PET) neuro-imaging to measure the rate at which we make serotonin in the brain.26 What they found was that men’s average synthesis rate of serotonin was 52% higher than that of women. This, and other research, has clearly shown that women are more prone to low serotonin. They also react differently. In women, low serotonin is associated with depression and anxiety, while in men, low serotonin is related to aggression and alcoholism. One possibility is our social conditioning: men `act out’ their moods, while women are more conditioned to `act in’ their moods.
What has been learnt about serotonin in the last few years is that there are a number of potential reasons for de®ciency, in addition to a lack of, or increased need for tryptophan:
. not enough oestrogen (in women)
. not enough testosterone (in men)
. not enough light
. not enough exercise
. too much stress, especially in women
. not enough co-factor vitamins and minerals.
If a person is suffering from low mood, feels tense and irritable, is tired all the time, tends to comfort eat, has sleeping problems and a reduced interest in sex, and some of the above apply, the chances are they are short on serotonin.
Low oestrogen means low serotonin and low moods.1 7 ,2 7 This is because oestrogen blocks the breakdown of serotonin. This may explain why women are more prone to depression premenstrually and in the menopause and thereafter. Low testoster- one has a similar effect in men.
Light also stimulates both oestrogen and serotonin and most of us do not get enough of it. The difference in light exposure outside and inside is massive. Most of us spend 23 out of 24 hours a day indoors, exposed to an average of 100 units (called lux) of light. That is compared to an outdoor level of 20 000 lux on a sunny day and 7000 lux on an overcast day. Now, more than ever before, many people rarely expose themselves to direct sunlight, and certainly not enough to maximise serotonin production. Of course, light de®ciency is worse in the winter.
Stress also rapidly reduces serotonin levels, while physical exercise improves stress response, and there- fore reduces stress-induced depletion of serotonin.
Is apathy a catecholamine deficiency?
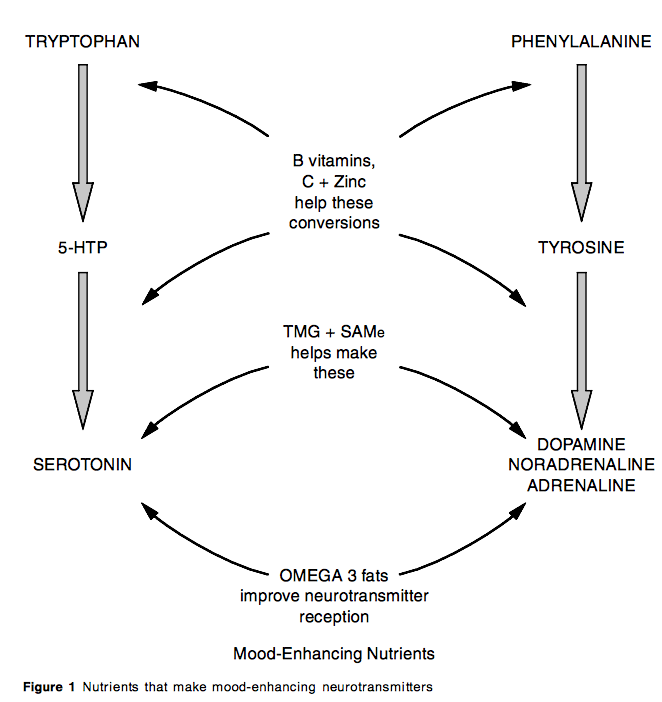
Another group of neurotransmitters associated with depression and lack of motivation are the catechola- mines ± dopamine, noradrenaline and adrenaline. As shown in Figure 2, both adrenaline and noradrenaline are synthesised from dopamine, which is made from the amino acid tyrosine, which is itself made from the amino acid phenylalanine. It is logical to assume that, if the drugs that block the breakdown of these neurotransmitters do elevate mood, then augmenting the amino acid phenylalanine or tyrosine might work too. And they do.
In a double-blind study by Helmut Beckmann and colleagues at the University of Wurzburg, Germany, 150 to 200 mg of the amino acid phenylalanine, or the antidepressant drug imipramine, were adminis- tered to 40 depressed patients for one month. Both groups had the same degree of positive results Ð less depression, anxiety and sleep disturbance.28 A group of researchers at the Rush Medical Center, Chicago, USA screened depressed patients by testing phenyl- ethylamine in the blood; low levels mean you need more phenylalanine. They then gave 40 depressed patients supplements of phenylalanine, and 31 of them improved.29
Tyrosine has been shown to work well in those with dopamine-dependent depression. In a pilot study administering 3200 mg tyrosine a day to 12 patients at the Hopital du Vinatier, France, a signi®cant im- provement in mood and sleep was observed on the very ®rst day.30
The military has long known that tyrosine improves mental and physical performance under stress. Recent research from the Netherlands demonstrates how tyrosine gives you the edge in conditions of stress. Twenty-one cadets were put through a demanding one-week military combat training course. Ten cadets were given a drink containing 2 g of tyrosine a day, while the remaining 11 were given an identical drink without the tyrosine. Those on tyrosine consistently performed better, both in memorising the task at hand and in tracking the tasks they had performed.31
In our clinical experience the best results are achieved by supplementing all of these amino acids ± 5-HTP, phenylalanine and tyrosine ± together with the B vitamins that help turn them into neurotrans- mitters, which are B6, B12 and folic acid.
B vitamins, methylation and depression
B vitamins act as co-factors in key enzymes that control both the production and balance of neuro- transmitters. For example, serotonin (5-HT) is pro- duced from 5-HTP by the addition of a methyl group (carboxylase), as is adrenaline from noradrenaline. This enzyme process is highly dependent on folate, as well as vitamins B1 2 and B6 . Folate de®ciency is extremely common among depressed patients. In a study of 213 depressed patients at the Depression and Clinical Research Program at Boston Massachusetts General Hospital, USA people with lower folate levels had more `melancholic’ depression and were less likely to improve when given antidepressant drugs.32 Very depressed people, and also those diagnosed with schizophrenia, are often de®cient in folate. A survey of such patients at Kings College Hospital’s psychiatry department in London, UK found that one in three had borderline or de®nite folate de®ciency. These patients then took part in a trial where they took folate for six months in addition to their standard drug treatment. Those given folate had signi®cantly improved recovery, and the longer they took the folate, the better they felt.33
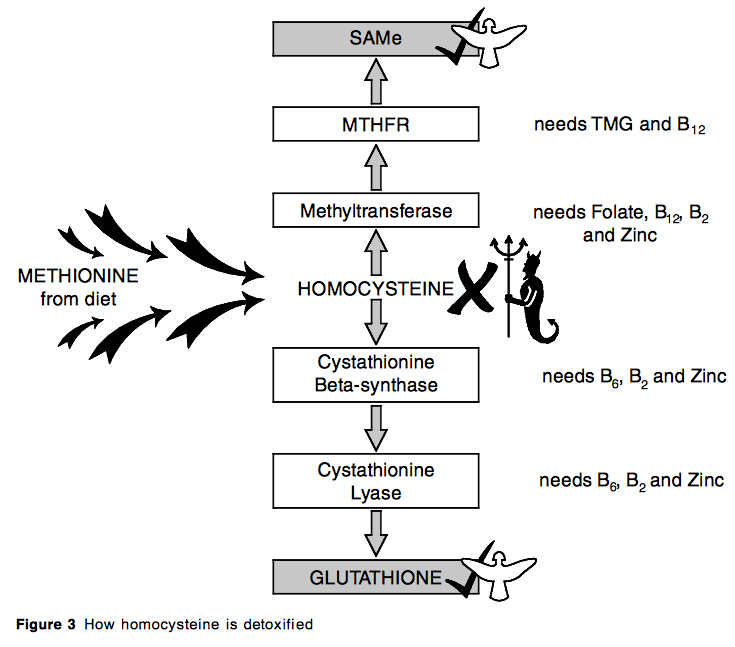
One current theory is that genetic differences worsening a person’s ability to methylate may both increase the tendency to depression (and schizophre- nia) and their need for folate, which may be better
re ̄ected by measuring homocysteine levels than by measuring blood levels of folate. This is because homocysteine is methylated `en route’ to s-adenosyl methionine (SAMe) by a folate-dependent enzyme methyl-tetrahydrofolatereductase, or MTHFR for short (see Figure 3). In one study, more than half (52%) of patients with severe depression were found to have elevated homocysteine and low levels of folate.34
Homocysteine levels are particularly high in patients with schizophrenia, even in the absence of dietary de®ciency in folate or vitamin B1 2 .3 5 When comparing 193 mixed-sex patients with schizophre- nia and 762 non-schizophrenic subjects, US research- ers found that average homocysteine levels were a very high 16.3 mmol/l for schizophrenics compared to 10.6 mmol/l in normal subjects.3 6 However, the dif- ference between groups was almost entirely attribut- able to the homocysteine levels of young male patients with schizophrenia. Genes, homocysteine and mental illness
Not everyone is born equal, as far as methylation is concerned. Around one in ten inherit a defective gene that means that the key methylating enzyme MTHFR does not work so well, increasing the need for folate, as well as vitamins B12, B6 and zinc. Vitamin B6 and zinc are involved because those with an MTHFR de®ciency accumulate homocysteine, which can also be detoxi®ed by conversion into cystathionine, via an enzyme dependent on pyridoxal-5-phosphate. Pyri- doxine (vitamin B6) is converted to pyridoxal-5- phosphate by a zinc-dependent enzyme. Supplement- ing a combination of folate, vitamin B12 and vitamin B6 has proven three times more effective at lowering homocysteine than folate alone.3 7 The combined ef®cacy of these nutrients for depression warrants investigation.
While folate de®ciency alone can induce depres- sion, the combination of de®ciency and a fault in the MTHFR gene is more likely to tip someone over into mental illness. To compensate for this, much higher levels of folate than normal are needed. According to researchers from Columbia University’s Department of Psychiatry in New York, USA this also applies to those with schizophrenia. They found increased levels of homocysteine, despite no apparent lack of dietary folate.3 8 The same is true for vitamin B1 2 . Many people with mental illness need more than a normal amount of vitamin B12 despite no obvious signs of de®ciency such as anaemia.39
A far better indicator of personal or individualised increased need for these B vitamins is a person’s homocysteine level.
SAMe and TMG: the master tuners
In Figures 2 and 3 you might have noticed these two strange-sounding nutrients. Both are kinds of amino acids. TMG stands for tri-methyl-glycine and SAMe stands for s-adenosyl methionine. Unlike the B vita- mins discussed above, which act as `methyl movers’, SAMe and TMG are methyl group donors. Both can lower homocysteine levels by donating methyl groups. Conversely, suf®cient folate, by enhancing the MTHFR enzyme, can increase production of SAMe.4 0 It is a two- way process.
SAMe is one of the most comprehensively studied natural antidepressants. Over 100 placebo-controlled, double-blind studies have shown that SAMe is equal
to or superior to antidepressants, works faster, most often within a few days (most pharmaceutical anti- depressants may take three to six weeks to take effect) and with few side effects.41±43 An intake of 200 to 600 mg a day is needed, but the trouble is that it is both very expensive and very unstable. A lot of SAMe sold in health food shops is pretty ineffective. An alternative that is much more stable and less costly is tri-methyl-glycine (TMG). In the body it turns into SAMe, but the supplement needed is three times as much ± 600 to 2000 mg a day, on an empty stomach or with fruit.
Mood-boosting fats
Omega-3 fats have a direct influence on serotonin status, probably by enhancing production and recep- tion. According to Dr JR Hibbeln, who discovered that ®sh eaters are less prone to depression, `It’s like build- ing more serotonin factories, instead of just increasing the ef®ciency of the serotonin you have’.44 Dr Basant Puri from London’s Hammersmith Hospital, UK re- ported the case of a 21-year-old student who had been on a variety of antidepressants, to no avail. He had a very low sense of self-esteem, sleeping problems, little appetite, found it hard to socialise and often thought of killing himself. After one month of supplementing ethyle-EPA (eicosapentaenoic acid), a concentrated form of omega-3 fats, he was no longer having suici- dal thoughts and after nine months no longer had any depression.4 5
Dr Andrew Stoll and colleagues at Harvard Medical School, USA ran a double-blind placebo-controlled trial of omega-3 fats, placing 14 adult manic depres- sives on the ®sh oils EPA and DHA (docosahexaenoic acid) and compared them with 14 taking an olive oil placebo. Both took the supplement alongside their normal medication. Those taking the omega-3 fats had a substantially longer period in remission than the placebo group. The ®sh oil group also performed better than the placebo group for nearly every other symptom measured.46 The Institute of Psychiatry in London is currently running a large double-blind trial with ®sh oils to further evaluate the effects of omega-3 fats on bipolar depression.
Omega-3 fats are effective for severe depression too. A recent trial published in the American Journal of Psychiatry tested the effects of giving 20 people suffer- ing from depression, who were already on antidepres- sants but still depressed, a highly concentrated form of omega-3 fat, ethyl-EPA, versus a placebo. By the third week, the depressed patients were showing major improvement in their mood, while those on placebo were not.4 7 Good mood foods and supplements
There is good logic, and substantial evidence that ensuring optimum nutrition in depressed patients can be highly effective. In addition to simple lifestyle changes such as encouraging exercise and outdoor activity to maximise light, reducing stress and recom- mending counselling, the following diet and supple- ment advice may help:
Diet
-
. Reduce sugar and stimulants (caffeinated drinks and smoking).
-
. Increase fruit and vegetables (five servings a day).
-
. Eat oily fish (mackerel, tuna, salmon, herring) at least twice a week.
-
. Ensure sufficient protein from fish, meat, eggs,beans and lentils.
Supplements
-
. B complex, including vitamin B6 10mg, folate 400mg and vitaminB12 10mg.
-
. Additional folate, 400 to 2000 mg a day.
-
. 5-HTP 200±300 mg a day.
-
. Omega-3-rich fish oil, two capsules a day, giving at least 400 mg of EPA.