Detecting and Treating Shoulder Impingement Syndrome. 충돌증후군의 진단과 치료 - 정리해야..
작성자문형철작성시간12.01.25조회수1,332 목록 댓글 3Dynamic scapular stabilization이 치료의 핵심이다.
충돌증후군은 Lack of scapular protraction(abduction), upward rotation, and posterior tilting
- 치료는 견갑골이 neutral position으로 자리잡도록 하는 것!!
panic bird...
![]() Detecting and Treating Shoulder Impingement Syndrome.PDF
Detecting and Treating Shoulder Impingement Syndrome.PDF
In Brief: The shoulder joint is most appropriately referred to as the "shoulder complex," since its total range of motion depends on four interworking articulations. The scapula is central in proficient shoulder activity, and rotator cuff muscles will not operate optimally if the scapula is poorly positioned. Dynamic scapular stabilization requires coordinated muscular activity, and muscle dysfunction will lead to glenohumeral incongruity during overhead athletic activities. Lack of scapular protraction(abduction), upward rotation, and posterior tilting can lead to subacromial impingement. Pain inhibition and fatigue can also provoke altered muscle patterns, but rehabilitation exercises can address biomechanic deficiencies.
- 어깨관절은 어깨관절복합체임. 어깨 움직임은 4개관절에 의존하여 rom이 완성되기 때문
- 견갑골은 능숙한 어깨움직임에서 중심에 있고, 회전근개 근육은 만약 견갑골이 중립자세에 위치하지 못하면 적절하게 작동하지 못함.
- 동적인 견갑골 안정성은 협응적 근육수축이 필요하고, 근육기능부전은 던지기 동작을 할때, 어깨 움직임의 불일치가 일어남.
- 견갑골 외전, 상방회전, 후방기울어짐 부족은 subacromial 충돌현상을 야기할 수 있음.
- 통증 억제와 피로는 근육움직임 패턴 변화를 초래하지만 재활치료는 생체역학적 불완전을 정상화 할 수 있음.
The shoulder "joint" is mobile and complex, serving as the functional link between the upper limb
and trunk when the upper extremity moves during functional tasks.1-5 Hence, the shoulder
complex must provide mobility with a stable base of support for the humerus. A relative absence of
bony constraints affords this range of motion (ROM) while sacrificing stability. Static and dynamic
soft-tissue restraints provide stabilization. The entire shoulder ROM is a function of the dynamic
interplay of four separate joints and their muscles and ligaments: the sternoclavicular,
acromioclavicular, glenohumeral, and scapulothoracic. Proper shoulder function results in total
mobility greater than that of any single articulation, and the structure should more correctly be
called the "shoulder complex."1-5
Shoulder complex dysfunction can arise when any of its components malfunctions. A common
presentation in overhead athletes can be impingement pain because of subacromial impingement
or anterior instability.3,6-8
The role of the scapula and, more important, scapulothoracic dyskinesis in secondary shoulder
impingement syndrome has been debated. Scapulothoracic kinematics have been well studied since
the 1940s, initially by Inman et al.9 Subsequent descriptive anatomic, neurophysical, and, more
recently, three-dimensional analyses have clarified normal and abnormal shoulder complex biomechanics. Clinicians should be aware of the ramifications of scapulothoracic dyskinesis when
evaluating patients who have shoulder pain and dysfunction.
Shoulder Anatomy and Physiology
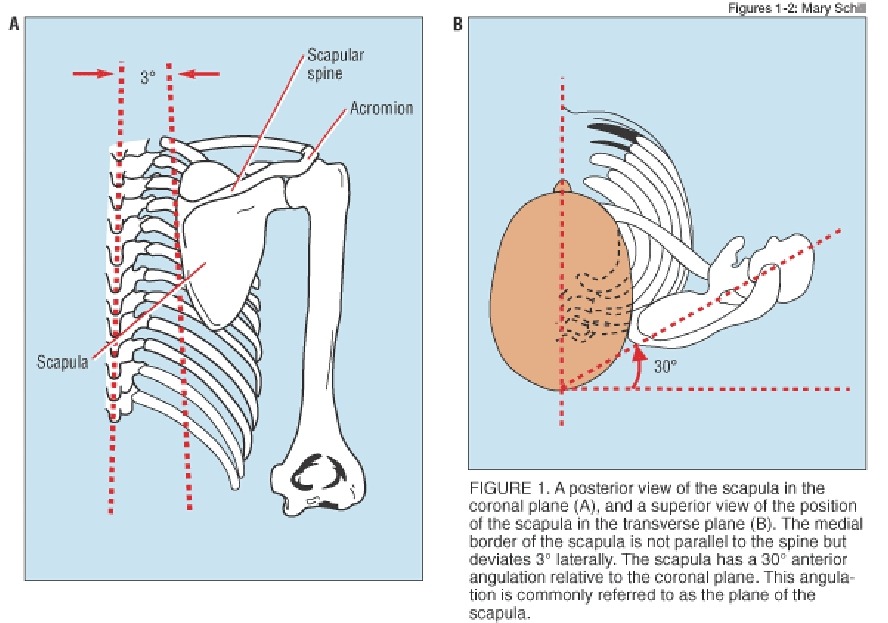
The scapulothoracic articulation (figure 1) incorporates a bone-muscle-bone juncture, with the acromioclavicular joint forming the only true synovial joint.1,3 This configuration allows for smooth gliding motions along the thoracic wall.1,3 The clavicle acts as a strut for the scapula, opposing the medially directed forces of the axioscapular muscles. This arrangement permits scapular rotation and translation along the thoracic cage.3
The shoulder complex muscles can be classified by anatomic and functional groupings.
The first anatomic group includes the axioscapular muscles that stabilize and rotate the scapula3: the trapezius, rhomboids, levator scapulae, and the serratus anterior.
The second anatomic group consists of the extrinsic shoulder girdle muscles: pectoralis major and minor,
deltoid, subclavius, biceps, triceps, and the latissimus dorsi.1,3
The final anatomic group consists of the rotator cuff muscles: supraspinatus, infraspinatus, subscapularis, and teres minor.3 The functional groupings are defined by agonists and antagonists working together as force couples
Force couples. The shoulder complex muscles can be classified by anatomic and functional groupings. The first anatomic group includes the axioscapular muscles that stabilize and rotate the scapula3: the trapezius, rhomboids, levator scapulae, and the serratus anterior. The second anatomic group consists of the extrinsic shoulder girdle muscles: pectoralis major and minor, deltoid, subclavius, biceps, triceps, and the latissimus dorsi.1,3 The final anatomic group consists of the rotator cuff muscles: supraspinatus, infraspinatus, subscapularis, and teres minor.3 The functional groupings are defined by agonists and antagonists working together as force couples.2,9 Movement. The glenohumeral joint ROM is central to the total ROM of the shoulder complex. In healthy patients, less than 1.5 mm of humeral head translation occurs on the glenoid fossa during
a 30° arc of motion.10 Therefore, in elevating the arm, the glenohumeral joint has an almost entirely rotational motion at the joint interface.1 Glenohumeral capsule redundancy allows for a wide ROM.
Capsular tightening from torsion provides a stabilizing moment at the extremes of ROM. During external rotation, the anterior capsule and the anterior band of the inferior glenohumeral ligament tighten. During internal rotation, the posterior capsule and posterior band of this ligament tighten. The posterior capsule plays a significant role in preventing anterior glenohumeral translation in abduction.1
Efficient arm elevation necessitates positioning of the humeral head within the shallow glenoid
fossa. Rotator cuff muscles plus the deltoid achieve this congruity. As the deltoid contracts, it
vertically displaces the humerus. The coupled inferomedially directed forces of the infraspinatus,
subscapularis, and teres minor counterbalance this upward force. The supraspinatus contracts to
facilitate glenohumeral abduction within the first 75°. As the moment arm of the deltoid improves
with further abduction, the supraspinatus compresses the humeral head into the glenoid with a
horizontal, medially directed force. The resultant greater force generated by the deltoid continues
to abduct the humerus above 90°.1,2,4 Changes in scapular position alter variables for torque about
the glenohumeral axis of rotation.
Healthy Scapular Biomechanics
The five individual roles of the scapula have been described by Kibler et al.2 Several different muscles facilitate protraction and retraction around the thoracic cage and upward rotation to elevate the acromion. These overlapping position changes help maintain glenohumeral congruity, keeping the joint as the instantaneous center of rotation (ICR) within the humeral head and preventing translation and soft-tissue strain. This mobile scapular platform accommodates the humerus in overhead activity, transmitting truncal energy to the upper limb.2,5 Hence, the scapula functions as the kinetic link between proximal segments and the energy released during a serve or pitch.
Scapulothoracic Kinesis in Arm Elevation
The rotations at the glenohumeral and scapulothoracic articulations are largely responsible for humeral abduction and flexion.1,3,4,6,9,10 The overall ratio of glenohumeral to scapulothoracic rotation is 2:1 throughout the full range of elevation. However, most movement occurs at the glenohumeral joint during the first 30° of abduction and the first 60° of flexion at a ratio of 4:1; then it continues at a ratio of 5:4.10
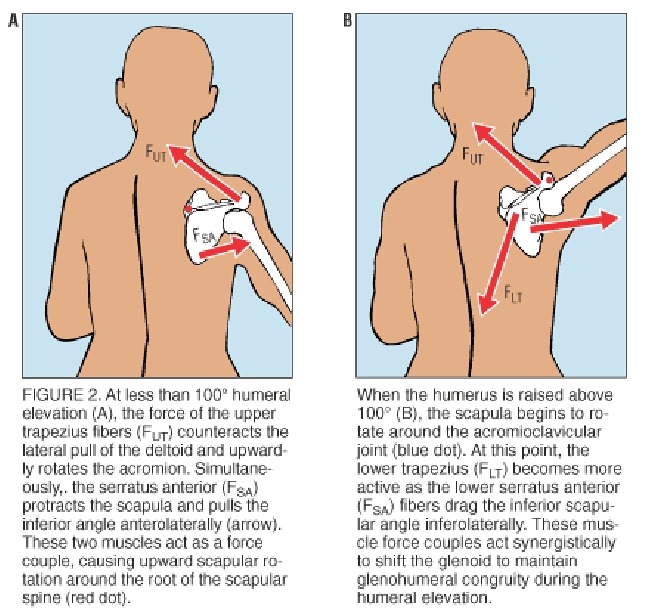
Elevation of the arm also induces a posterior scapular tilting that is defined as the superior scapula and acromion moving away from the greater tuberosity of the humerus while the inferior scapular angle moves toward the rib cage.1,11-13 Such scapular tilting is more prominent during the first 90° of elevation.1,11 ICR movement. Several investigators have demonstrated that the scapular ICR during arm elevation is initially located at the root of the scapular spine during the first 90° to 100° of
elevation (figure 2A). The ICR progresses to the acromioclavicular joint as elevation continues above 100°, and this action has been supported by radiologic studies.4
During elevation, the upper trapezius is activated to oppose the lateral pull of the deltoid. The superior fibers of the serratus anterior are activated to maintain proximity between the scapula and thoracic cage and to oppose the pull of the deltoid muscle (figure 2B).
Simultaneously, the rotator cuff muscles are firing to maintain the ICR of the glenohumeral axis, thus exerting a lateral force on the scapula. The combined lateral torque of the serratus anterior and rotator cuff is counterbalanced by the levator scapulae, rhomboids, and lower fibers of the trapezius.14-17 Thus, the lower fibers of the serratus anterior are free to drive the inferior scapular angle laterally, achieving upward scapular rotation about an imaginary axis extending from the sternoclavicular joint to the point of the root of the scapular spine.4,9,14,17,18
ICR and force couples.
The rotation about the sternoclavicular and root of the scapular spine axis continues until approximately 100° of glenohumeral abduction, at which point the costoclavicular ligament becomes taut, restricting further upward rotation about this axis. As the serratus anterior continues to contract, the root of the scapular spine glides inferolaterally as the scapula follows its trajectory along the slope of the rib cage.
Consequently, the root of the scapular spine can no longer remain stationary, and so the ICR shifts
to the acromioclavicular joint (see figure 2B).1,4,14 Then, the roots of the scapular spine and
scapular inferior angle move radially about the acromioclavicular joint until the trapezial ligament
becomes taut, restricting further anterolateral excursion of the scapula. At this point, the humeral
head is positioned superior to a stable base provided by the glenoid fossa.1,4,14
Abnormal Biomechanics and Impingement Syndrome
Differing views exist about causes of shoulder pain, instability, and impingement. Jobe et al6
suggest that mild anterior glenohumeral instability is a consequence of the progressive attenuation
of the static anterior stabilization structures from repetitive throwing. An injurious cycle ensues,
with fatigue of dynamic stabilizers leading to further glenohumeral anterior translation and
encroachment of the coracoacromial arch.6,7,19
Factors affecting scapular orientation. Scapular malrotation could predispose patients to
coracoacromial arch impingement3 and derive from poor scapular positioning in overhead athletic
activities.2 Many influences serve to disrupt scapulothoracic rhythm, including pain, soft-tissue
stress, and glenohumeral capsular tightness. Typically, muscle dysfunction results from blunt
traumatic injury or microtrauma-induced strain and fatigue. Other conditions, such as labral lesions
or arthrosis, can lead to pain-inhibited muscle weakness2,16,20 and, in turn, produce poor
coordination of shoulder girdle muscles and provoke inefficient scapular stabilization and less
torque generation.2,16
Evidence for a scapular role. Descriptive anatomic studies have characterized the relationship
between scapular positions and changes in the subacromial space.21-23 Magnetic resonance
imaging (MRI) demonstrated a relative decrease in the subacromial space in the sagittal plane with
passive scapular protraction in healthy shoulders.21 Thus, without acromial elevation, the humerus
approaches the inferior surface of the acromion with the arm in 0° elevation. During active
abduction in the scapular plane, patients who had shoulder impingement syndrome (SIS) without
MRI evidence of rotator cuff tears or acromioclavicular joint pathology demonstrated reduced
acromiohumeral and claviculohumeral distances relative to passive abduction.22
That these observations were made with active arm elevation rather than passive arm elevation
points to disrupted force couples as a cause. The lack of anatomic evidence of structural injury to
the rotator cuff supports the notion that dyssynergic activity of the shoulder girdle muscle
contributes to SIS.19
Shoulder and muscular deficits. Using Moire topography, Warner et al23 documented a relative
asymmetry between the scapulae of shoulders with SIS and healthy contralateral shoulders. These
asymmetries were more pronounced during dynamic arm descent from glenohumeral flexion at
90°. All the patients with SIS demonstrated abnormal scapulothoracic rhythm, and none of the
subjects had rotator cuff tears. The observation that abnormal scapulothoracic rhythm was
significantly worse during eccentric activity of the scapular stabilizers strengthens the argument
that scapulothoracic dyskinesis is integral in SIS.
Those with glenohumeral instability who had various labral lesions also demonstrated abnormal
scapulothoracic movement. Scapulothoracic dyskinesis is present in conditions such as labral
lesions; thus, painful shoulder conditions may disrupt scapulothoracic rhythm, leading to secondary SIS.3,20
Posterior glenohumeral capsule tightness has been documented clinically and experimentally in
patients with SIS.19,23,24 An elevated and protracted scapular position may be a compensatory
effort to provide functional glenohumeral internal rotation. In athletes who use overhead arm
movements, anterior glenohumeral strain and subacromial impingement arise as the scapula
becomes more protracted and less able to rotate upward.3,6,25
Altered muscle firing. Methodical studies have identified altered muscle firing patterns as integral
in SIS. McQuade et al26 studied healthy subjects and confirmed that fatigue of the axioscapular
muscles can result in a destabilized scapula during humeral elevation. Myoelectric signs of fatigue
in the upper and lower trapezius and serratus anterior corresponded with a 50% decrement in peak
force-generating capacity. The scapular stabilizers are active during humeral elevation and thus are
susceptible to fatigue, resulting in altered scapulothoracic kinematics.
Ludewig and Cook27 showed that patients with SIS had increased activation of the upper and lower
trapezius and decreased serratus anterior activity compared with patients without SIS. This finding
suggests that the trapezius muscle alterations attempt to compensate for the decreased serratus
anterior activity to achieve upward scapular rotation. However, the trapezius activity increases
were inadequate for posteriorly tilting the scapula during arm elevation.27 Glousman et al16
detected similar muscle findings in throwing athletes with anterior stability.
Scapular tilting. Several studies11-13,27,28 document a relative lack of posterior scapular tilting in
SIS patients. The relative anteriorly tilted scapular position seems to predispose patients to SIS12
by causing functional stenosis of the coracoacromial joint. These findings were confirmed by Hebert
et al,11 who studied the frontal plane in arm abduction in SIS.
Disruption of the serratus anterior–trapezius force couple allows the inferomedial scapular angle to
"float" slightly away from the thoracic cage, causing the acromion to tilt toward the greater
tuberosity.11 The greater the decrease in posterior tilting, the greater is the disability.11 Only one
small statistically significant difference between the affected and healthy shoulders was detected.
However, a large percentage of both shoulders in these patients had scapular rotation amplitudes
outside the range of healthy shoulders, suggesting that abnormal scapulothoracic kinetics precede
the clinical signs and symptoms of SIS. Thus, scapulothoracic dyskinesis may be a risk factor for
developing serratus anterior impingement.11
Clinical Evaluation of Scapulothoracic Rhythm
The clinician should understand the integration of the shoulder complex into the kinetic chain and
fully evaluate all factors that can affect scapular function. Thoracic kyphosis can cause relative
scapular protraction, and excessive cervical lordosis can alter protraction and retraction.3,29
Oblique pelvic tilts, leg-length discrepancies, and excessive lumbar lordosis can alter the transfer of
forces at the shoulder complex.3
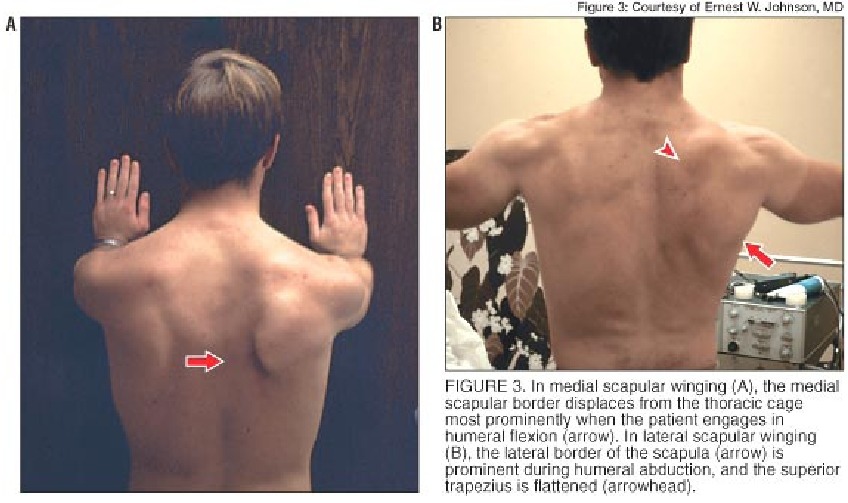
Medial and lateral winging. The physician should observe scapular position with the patient at
rest and look for obvious winging. Mediosuperior winging is typical of pure serratus anterior paresis
consistent with a long-thoracic nerve injury (figure 3A). Trapezius weakness will manifest as lateral
winging with an elevated acromion suggestive of spinal accessory nerve injury (figure 3B). The
physician should continue to observe as the patient elevates the arm in both flexion and abduction
in the frontal plane and look for asymmetry, especially in the descending phases.
Recently, Kibler et al28 have documented three distinct patterns of scapulothoracic dyskinesis. Type
1 scapulothoracic dyskinesis manifests prominence of the inferomedial scapular border, type 2
exhibits prominence of the entire medial scapular border, and type 3 is characterized by superior
medial border prominence.28 One can manually assist the symptomatic side by applying upward
and laterally directed force to the inferior angle of the scapula and assessing for amelioration of
impingement symptoms.3,8 A provocative maneuver can be used to assess the scapular stabilizers'
conditioning: A patient's inability to pinch the scapulae together in retraction for more than 15
seconds before experiencing muscular burning suggests premature fatigue of these muscles.3
Lateral slide test. This reliable and reproducible test can quantitatively measure scapular
asymmetry and accurately evaluate the moving scapular landmarks and scapular muscles.3 The
examiner measures the distance between the inferior angle of the scapula and the adjacent
spinous process in three different arm positions: (1) with the arm at the side, (2) with the patient's
hand on his or her iliac crest, and (3) with the arm abducted 90° in the coronal plane.
Shoulders of healthy patients show decreased asymmetry as they progress from the first to third
position. However, in injured shoulders, the asymmetry persists and increases, with a difference of
1.5 cm or more indicating an abnormality.3 Moire topography is more sensitive than physical
examination for detecting asymmetric scapular positions, but this technique is much less practical,
because it requires special equipment and trained personnel.3,23
Restoration of Normal Scapulothoracic Kinesis
Successful rehabilitation of shoulder disorders addresses all the abnormalities discovered during the physical examination.3 Lumbar or thoracic strength deficits must be addressed with
strengthening exercises for trunk flexors, extensors, and rotators. Postural abnormalities and
anteroposterior and rotational inflexibilities must be corrected, and efficient biomechanics must be
restored.3,5 These exercises can overlap the initiation of scapulothoracic exercises.
Guiding rehabilitation. Scapular rehabilitation is divided into three stages: stability exercises,
closed-chain exercises, and open-chain exercises.2,3 Initially, external assistance with scapular
control can alleviate impingement pain, assist the function of the scapular stabilizers, and reduce
injurious stretching of important stabilizing muscles.3,8 Such devices include taping techniques and
posterior support braces such as figure-eight clavicle collars.3,8 These devices help restore normal
positioning and stimulate coordination of muscle firing patterns.3,15 Isometric exercises such as
scapular pinch and shrug are introduced in sets of low repetitions (three to five) to reduce overload
stress and to encourage repair.3,8
Closed–kinetic-chain activities provide the most physiologic way to reestablish normal motor firing
patterns.3 The patient uses the wall and, when exercising on all fours, uses the floor and moves
through scapular elevation, depression, protraction, and retraction with the arm at 90° elevation
and the elbow extended. This positioning best simulates normal functional patterns and elicits
physiologic patterns of shoulder girdle muscle co-contractions.3
Once these exercises are mastered, the patient can progress to more complex movements. Some
researchers17 suggest the use of four core exercises to target the scapular stabilizers: scaption
(humeral elevation in the scapular plane), rowing, push-ups with terminal scapular protraction, and
press-ups.
Moseley et al17 observed peak activity of the serratus anterior during glenohumeral flexion,
scaption with glenohumeral internal rotation, and abduction. The inferior serratus anterior fibers
exhibited peak activity at the bottom of the push-up with terminal protraction movement.17
Therefore, emphasis of the eccentric component of scapular movement as the chest nears the floor
is pertinent.
Progression and return of function. Once patients establish foundations with the isometric and
closed-chain activities, they can progress to open-chain exercises. Restoration of healthy
scapulothoracic rhythm is required for progression. If less than 1 cm of asymmetry is present
between the inferior angles in the third position and the scapula ascends and descends smoothly
during arm elevation, then scapular stability has improved.3
Open-chain exercises incorporate proprioceptive neuromuscular facilitation patterns and plyometric
activities to condition the scapular stabilizers for return to play or other functional activities.
Plyometric muscle activities, such as throwing an air-filled ball, provide dynamic stabilization
challenges to the shoulder complex muscles. These conditioning and retraining activities restore
the scapulothoracic kinetics for sport-specific or functional activities.2,3 Once the scapular base has
been stabilized, patients can transition to restorative training for rotator cuff muscles.
The Rehabilitative Wrap
Evaluating the relative contribution of scapulothoracic dyskinesis can be elusive. Assessing the
predisposing shoulder complex characteristics is imperative to obtaining functional restoration. The musculoskeletal specialist should always start with the scapular base in patients who have shoulder
pain. Only after proficient scapular stabilization is restored should treatment focus on rotator cuff
or distal upper-limb dysfunction.