어깨 관절의 불안정성에 관한논문
![]() Shoulder Instability. management and rehabilitation.pdf
Shoulder Instability. management and rehabilitation.pdf
abstract
Shoulder dislocation and subluxation occurs frequently in athletes with peaks in the second and sixth decades. The majority (98%) of traumatic dislocations are in the anterior direction. The most frequent complication of shoulder dislocation is recurrence, a complication that occurs much more frequently in the adolescent population. The static (predominantly capsuloligamentous and labral) and dynamic (neuromuscular) restraints to shoulder instability are now well defined. Rehabilitation aims to enhance the dynamic muscular and proprioceptive restraints to shoulder instability. This paper reviews the nonoperative treatment and the postoperative management of patients with various classifications of shoulder instability.
- 운동선수의 어깨 탈구, 아탈구는 20대, 60대에 가장 많이 발생. 98%에서 ant direction으로 타박에 의한 탈구.
- 어깨 탈구의 흔한 합병증은 반복재발
- 어깨불안정성에 정적( capsuloligamentous and labral), 동적(neuromuscular) 제한은 잘 정의되어 있음
- 재활치료의 목표는 어깨불안정성에 dynamic muscular and proprioceptive restraints을 증진시키는 것
Shoulder stability is the result of a complex interaction between static and dynamic shoulder restraints. Disruption to these restraints manifests itself in a spectrum of clinical pathologies ranging from subtle subluxation to shoulder dislocation. This article describes the anatomical variants associated with both traumatic and atraumatic shoulder instability and evaluates existing literature pertaining to nonoperative and surgical management with the ultimate aim of providing guidelines for the rehabilitation of various classifications of shoulder instability.
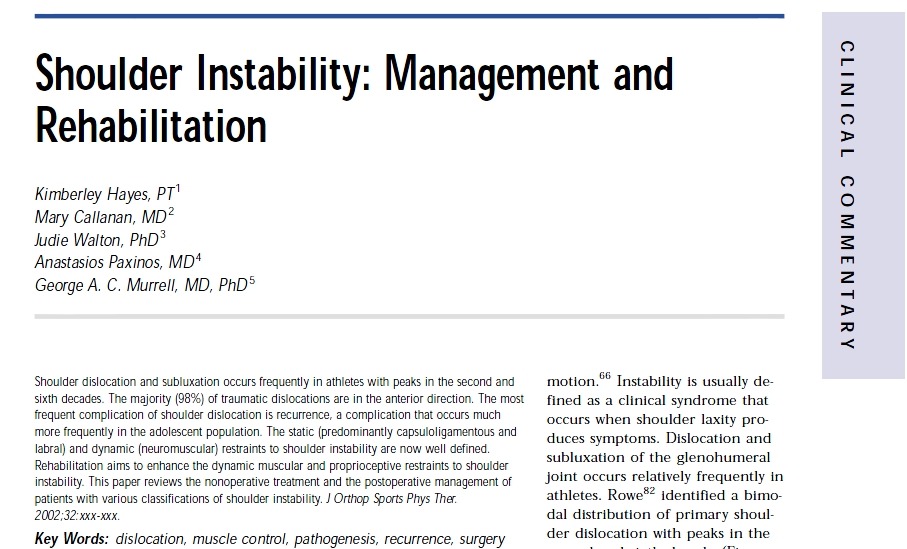
Primary dislocation
- 20대와 60대에 가장 많이 발생
- 95%에서 trauma가 원인. 98%가 ant direction.
- 5%에서 atraumatic origin. 원인은 capsular laxity or altered muscle control of the shoulder complex.
Recurrent dislocation.
- primary dislocation의 중요한 합병증은 recurrent dislocation. 2년이내에 대개 다시 탈구가 발생.
- 재탈구는 대개 나이가 들어감에 따라 탈구는 줄어들고 젊은 경우 탈구가 많음.
Functional Anatomy and Biomechanics
Static shoulder restraints refer to the bony ball and socket configuration of the shoulder and the major soft tissues holding these bones together. The soft tissues include the capsule, the glenohumeral ligaments and the glenoid labrum. Dynamic shoulder restraints refer to the neuromuscular system, including proprioceptive mechanisms and the scapular and humeral muscles.
Static Stabilizers
While the shoulder joint surfaces are highly congruent,89 there is minimal bony containment of the humeral head in the glenoid cavity. At most, only 25% of the humeral head is in contact with the glenoid fossa in any given shoulder position. 13 Under normal circumstances the shoulder capsule is relatively large and loose.19
- shoulder joint surfaces가 가장 적합할때, glenoid cavity에 humeral head의 bony 견제가 최소로 존재
- humeral head의 오직 25%가 glenoid fossa에 접촉. 정상적인 상황에서 shoulder capsule은 상대적으로 크고, loose함.
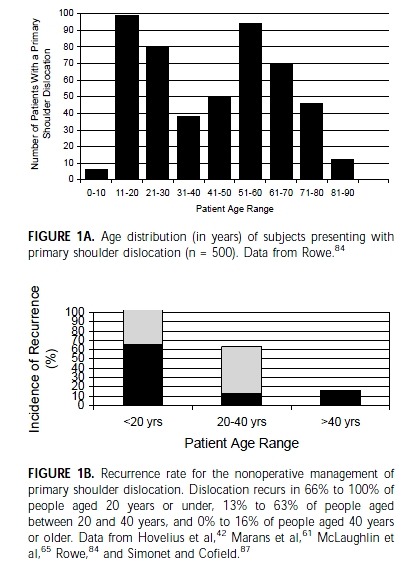
The discrete thickenings or capsular ligaments of the capsule have been named the superior glenohumeral ligament (SGHL), the middle glenohumeral ligament (MGHL), and the inferior glenohumeral ligament complex (IGHLC) (Figure 2).72 The relative contributions of the capsuloligamentous restraints to stability of the glenohumeral joint are variable.
어깨 인대의 기능
1) The SGHL primarily limits anterior and inferior translation of the adducted humerus.15,72
2) The MGHL primarily limits anterior translation in the lower and middle ranges of abduction.15,72
3) The IGHLC is the longest and strongest of the glenohumeral ligaments85 and has been identified as the primary static restraint against anterior, posterior, and inferior translations when the humerus is abducted beyond 45°.72
The labrum constitutes the fibrocartilagenous rim of the glenoid. Inferiorly it is firmly attached to the glenoid, although it may be loose and mobile anterosuperiorly. Although variable in size, the labrum contributes to shoulder stability by increasing the depth of the glenoid cavity from an average of 4.5 to 9.0 mm in the superior-inferior direction and from an average of 2.5 to 5.0 mm in the anteriorposterior direction.43 The labrum may also act as a chock block(멈추개), having been shown to increase resistance to glenohumeral translation by up to 20%.58,63 The labrum provides attachment of the glenohumeral ligaments anteriorly, and the biceps tendon superiorly.
- 관절순은 glenoid의 fibrocartilagenous rim (섬유인대 림).
- 관절순은 위로는 상완이두근 건이 부착하고, 아래로는 glenohumeral ligament가 부착.
Dynamic Stabilizers
A number of dynamic EMG studies have shown that the rotator cuff works in a combined synergistic action to create a compressive force at the glenohumeral joint during shoulder movement.16,45,55 Radiographic evaluation of glenohumeral kinematics in the normal shoulder has shown that the center of the humeral head deviates from the center of the glenoid fossa by no more than an average of 0.3 mm throughout abduction in the plane of the scapula.22,79 With fatigue of the rotator cuff and deltoid muscles, there was an average 2.5 mm superior migration of the humeral head.22
- 회전근개 근육은 어깨 움직임 동안 GH joint에서 주요 작용을 함
- 회전근개(극상근, 극하근, 소원근, 대원근)와 삼각근의 근피로는 humeral head의 평균 2.5mm 상방이동
The biceps assist the rotator cuff in creating glenohumeral joint compression. In an abducted and externally rotated cadaveric shoulder model,46 static loading of the rotator cuff and biceps brachii muscle (long and short heads) significantly reduced the magnitude of simulated anterior humeral head translation. For conditions of increasing shoulder instability (vented capsule, simulated Bankart lesion) the biceps brachii made a greater contribution to shoulder stability than the individual muscles of the rotator cuff.46
- 상완이두근은 GH joint 압박력을 창조하는데 회전근개를 도움.
- 어깨관절의 불안정성이 증가된 상황에서 상완이두근은 회전근개보다 어깨관절의 안정성을 제공하는 역할을 함.
The individual tendons of the rotator cuff splay and interdigitate to form a wide, continuous insertion on the humeral tuberosities.23 Near their insertions, the deep surface of these tendons are tightly adherent to the underlying joint capsule.23,24 It has been hypothesized that contraction of the rotator cuff muscles may tighten the underlying capsule, creating a soft tissue barrier to excessive humeral head translation.104,105
EMG studies of shoulder kinematics have shown that the scapulothoracic muscles operate as functional units to create upward scapular rotation.9,45 Synchronous scapular rotation and humeral elevation is prerequisite for maintaining optimal alignment of the glenoid fossa and humeral head.45 Because there are no scapulothoracic ligamentous restraints, the
scapulothoracic muscles also serve to stabilize the scapula on the thorax. Stability of the scapula in relation to the moving upper extremity provides a secure platform for the glenohumeral articulation and the action of attaching humeral muscles.
- 근전도 검사에 의하면 scpulothoracic muscle은 견갑골의 upward rotation을 담당하는 기능적 단위가 됨.
- 조화로운 견갑골 회전과 상지 거상은 humeral head와 glenoid fossa의 최적의 정렬을 유지하는 전제조건임
- capulothoracic ligamentous restraints이 없기 때문에 scapulothoracic muscles은 흉곽에 견갑골을 안정화시키는 역할
It has been suggested that proprioceptive mechanisms involving reflexive muscular action may protect against excessive translations and rotations of the glenohumeral joint.100 A recent histological investigation97 has demonstrated the presence of mechanoreceptors (ruffinian corpuscles and pacinian corpuscles) within the capsuloligamentous restraints of
the shoulder. These specialized nerve endings relay afferent information relating to joint position and joint motion awareness (proprioception) to the central nervous system.
- 반사성 근육 활성과 관련된 고유수용성 기전은 GH joint의 과도한 이동과 회전을 방어하는 역할
The perceived sensation of shoulder joint position and movement is likely to play an important role in coordinating muscular tone and control. It has been suggested that joint instability secondary to trauma may be associated
with a decrease in proprioceptive reflexes and thus a predisposition to subsequent reinjury.97
- 어깨관절 위치감각과 운동감각은 근육톤과 조절을 coordinate하는데 중요한 역할.
Traumatic Anterior Dislocation
Mechanism of Injury The most common mechanism
of anterior shoulder dislocation has been described
as forced external rotation and abduction of the humerus
as seen in a basketball player who attempts to
block an overhead pass.5,59 Other mechanisms of injury
have included a fall onto an elevated outstretched
arm and direct force application to the
posterior aspect of the humeral head.5,59
Sequelae of Anterior Dislocation There are several
morphological changes associated with anterior dislocation
of the glenohumeral joint. The most significant
in terms of recurrent instability are those associated
with the inferior glenohumeral ligament
complex and its attachments to the labrum and humerus.
In 1923 Bankart8 described anterior labral
detachment as the essential lesion in traumatic anterior
instability (Figure 3). Rowe and Zarins84 noted
the lesion in 85% of traumatic instability cases requiring
surgery. An osseous Bankart defect on the
antero-inferior glenoid rim is best appreciated radiographically
with a West Point view.73 Detachment of
the anterior labrum and plastic deformation of the
capsule and inferior glenohumeral ligament complex10
contribute to increased anterior humeral
translation.44,90
The most common bony lesion associated with
traumatic glenohumeral instability is a compression
fracture at the posterolateral margin of the humeral
head. This occurs as the humeral head impacts into
the glenoid edge during dislocation and has been
termed the Hill Sach’s lesion.39 This lesion has been
reported to occur in over 80% of traumatic instability
cases21,73,99 and is best appreciated radiographically
with a Stryker Notch view and an
anteroposterior view with the shoulder in internal ㅜrotation.73 The lesion must involve more than 30%
of the proximal humeral articular surface to play a
significant role in recurrent instability.90 The lesion is
smaller than this in the majority of cases of traumatic
shoulder instability.83,99
Scapulothoracic motion asymmetry, as determined
by Moire topographic evaluation, has been found in
64% of patients with antero-inferior shoulder instability
compared to 18% of subjects with normal shoulders.
101 In 36% of patients with antero-inferior instability,
this asymmetry presented as scapular winging,
hence an increased anterior orientation of the
glenoid with repeated shoulder elevation. Simulated
glenoid anteversion in the abducted and externally
rotated shoulder has been shown to significantly increase
in situ strain of the anterior band of the inferior
glenohumeral ligament.102 Regardless of whether
scapulothoracic motion asymmetry represents a cause
or an effect of shoulder instability, suboptimal
glenohumeral joint alignment implies an increased
loading of surrounding capsuloligamentous restraints.
Proprioceptive deficits have been shown for patients
with traumatic anterior shoulder instability.88,10
Warner et al100 reported a significantly greater
threshold to detection of passive shoulder motion for
patients with shoulder instability compared to subjects
with normal shoulders (2.8° angular displacement
versus 1.9° angular displacement before detection
of passive shoulder motion). Reproduction of a
joint reference position was also significantly less accurate
for subjects with shoulder instability.100 Interestingly,
in this same study, a third group of test subjects
who had undergone arthroscopic or open
Bankart repair demonstrated normal proprioceptive
function for both of the variables examined.
Capsulolabral integrity may thus be important for
normal proprioceptive function.
Age-Related Changes
The high incidence of recurrent shoulder dislocation
in the adolescent population as opposed to recurrence
in those over 40 years of age may be explained,
in part, by the collagen profile of
encapsulating shoulder tissues. Collagen is the major
protein of ligaments and tendons. In newborns,
soluble collagen (type III) is synthesized and the fibers
formed from collagen type III are supple and
elastic. With each passing decade, collagen-producing
cells make less soluble collagen and progressively
convert to synthesizing an insoluble, more stable type
I collagen (Figure 4). This form of collagen has sulfur
groups that have a high tendency to cross-link
and form bridges between the collagen filaments,
causing the fibers they comprise to be relatively
tough and nonelastic. This changing ratio of collagen
types I and III throughout the body is so reliable
that chronological age of an individual can be
determined by analyzing the collagen type III content
of a skin sample according to the following
equation:7 collagen type III (mg)/wet dermis
(gm) = 1.3e-Age/23.5. Thus, the higher content of
stretchy collagen in tendons and ligaments can help
to account for the observation that younger people
who have already had a dislocated shoulder are
much more prone to recurrent dislocation than
older people. Once excessively stretched, their capsule
and ligaments may be too loose to provide the
secure and stable shoulder support required for
maximum athletic performance.
Atraumatic Dislocation
A small group of patients dislocate or sublux their
shoulders with minimal force application or by putting
their arms into certain positions. Neer and Foster70
thought the pathological entity was a loose re-dundant inferior capsule and introduced the term
multidirectional instability. Multidirectional instability
is less often associated with a labral detachment or
Bankart lesion. The condition is associated with generalized
ligamentous laxity.3,70
The definitive etiology of atraumatic instability is
still not clear and it may be multifactorial. Current
etiological theories include suboptimal muscle control
for shoulder function, a deficiency in the rotator
cuff interval, and connective tissue abnormalities.
EMG analyses of shoulder motion have demonstrated
altered patterns of shoulder muscle activity
for patients with atraumatic anterior instability when
compared to normal subjects.56 Radiographic analyses
of glenohumeral kinematics in patients with
atraumatic multidirectional instability have demonstrated
an increase in humeral translation and a decrease
in upward rotation of the glenoid fossa for
scapular plane abduction when compared to normal
subjects.75 While these studies have shown a correlation
between abnormal shoulder muscle activity,
glenohumeral incongruence and scapulohumeral
motion asymmetry, it remains to be determined
whether these findings represent a cause or an effect
of atraumatic shoulder instability.
Clinical studies have documented an association
between the size of the rotator cuff interval (a defect
in the anterosuperior capsule between the superior
border of the subscapularis tendon and the anterior
margin of the supraspinatus tendon) and the
amount of anterior84 and inferior glenohumeral
translation.71 A biomechanical study using a
cadaveric shoulder model has confirmed the importance
of the anterosuperior capsule in preventing
inferior subluxation of the adducted shoulder.36 A
large rotator cuff interval has been viewed by some
authors as a possible causal mechanism in some cases
of atraumatic shoulder instability.
Rodeo et al81 analyzed the collagen and elastic fibers
in the shoulder capsule in patients with unidirectional
anterior instability, multidirectional instability
at primary surgery, multidirectional instability at
revision surgery, as compared to patients with no history
of instability. Skin analysis between these groups
demonstrated a significantly smaller mean collagen
fibril diameter in skin samples in the primary
multidirectional instability group compared with the
unidirectional anterior instability group. This suggests
the possibility of an underlying connective tissue
abnormality.
Acquired Shoulder Instability
Chronic stress associated with repetitive overhead
sports has been cited as a predisposing factor to anterior
shoulder instability.1,2,31,57 These athletes usually
perform activities such as throwing, volleyball,
and tennis, all of which require extreme external
rotation with the humerus abducted and extended in
the horizontal plane. A current hypothesis is that
repetitive glenohumeral capsular overload in this position
of extreme range of motion leads to gradual
attenuation of the antero-inferior static restraints,38,57
increased glenohumeral translation and a continuum
of shoulder pathology.57 On the basis of arthroscopic
observations, Kvitne and Jobe57 described a pattern
of injury in this athletic population that involved primary
instability and secondary subacromial impingement
or posterosuperior glenoid impingement of the
undersurface of the rotator cuff with the posterosuperior
glenoid rim. In a separate retrospective review
of arthroscopic findings for 61 throwing athletes,
Nakagawa et al69 reported anterior joint laxity
in 33% of patients, detachment of the superior
glenoid labrum in 51% of patients, posterior labral
injury in 80% of patients, and rotator cuff tears in
66% of patients. While this study confirmed the presence
of several different shoulder pathologies in this
athletic population, there was no correlation among
anterior joint laxity, superior or posterior labral injury,
and a rotator cuff tear.
Nonoperative Management of Dislocation
Traumatic Instability Various treatments, including
shoulder immobilization, activity restriction, and exercise
rehabilitation have been advocated in the
management of primary traumatic anterior shoulder
dislocation. While low recurrence rates have been
reported for this condition for conservatively managed
older patients, the prognosis for patients aged
20 years and younger is generally considered to be
poor.
In a prospective study of 257 patients (age range
12 to 40 years) with a primary traumatic anterior
shoulder dislocation, Hovelius et al42 found no difference
in redislocation rates between treatment with
early mobilization and treatment with 3 to 4 weeks of
immobilization. Regardless of the immobilization period,
redislocation occurred in 47% of patients aged
from 12 to 22 years, 34% of patients from 23 to 29
years, and 13% of patients aged from 30 to 40 years
for the 2-year duration of the study.
Other studies of primary traumatic anterior shoulder
dislocation performed retrospectively have found
no beneficial effect of immobilization of up to 6
weeks duration.61,87 In one study of 21 patients (age
range 4 to 16 years), 100% recurrence rates were
reported for immobilization periods that included 0,
4, and 6 weeks in duration.61 Another study of 116
patients (age range 14 to 96 years) reported an overall
redislocation rate of 33% with no difference in
recurrence for periods of immobilization between 0
and 6 weeks duration.87 In the same study, 82% of
athletes aged 30 years or younger sustained a
redislocation (all due to athletic injury) compared to
30% of nonathletes of similar ages. While the type or
length of shoulder immobilization had no influence on the rate of recurrence, significantly better results
were reported for patients aged 30 years or younger
with 6 to 8 weeks of activity restriction compared to
activity restriction of less than 6 weeks in duration
(resolution of symptomatic shoulder instability in
56% and 15% of patients, respectively).
Therefore, the literature does not support shoulder
immobilization with a traditional sling in the
nonoperative management of primary traumatic anterior
shoulder dislocation. In a recent study47 of 18
patients who underwent magnetic resonance imaging
between 1 and 60 days after traumatic anterior dislocation
(6 patients with a primary dislocation, 12 patients
with recurrent dislocation), better approximation
between the Bankart lesion and the glenoid
neck occurred with the humerus positioned in adduction
and external rotation as compared to that
which occurred with conventional immobilization in
a position of humeral adduction and internal rotation.
In support of this finding, a cadaveric shoulder
experiment37 involving similar humeral positions (adduction
and external rotation versus adduction and
internal rotation) and a simulated Bankart lesion,
demonstrated significantly greater contact force between
the detached glenoid labrum and the glenoid
neck with the arm in the externally rotated position.
Lack of capsulolabral and glenoid contact after
glenohumeral joint dislocation helps to explain the
observation in previous studies that the rate of recurrence
is not influenced by the method or duration
of shoulder immobilization.47
There have been few studies investigating outcomes
for exercise rehabilitation in the nonoperative
management of primary traumatic anterior shoulder
dislocation. In one prospective study6 of 20 male patients
(age range 18 to 22 years), Aronen and Regan
reported a return to unrestricted duty and sports
participation without redislocation for 75% of cases
with a rehabilitation program that emphasized
strengthening for the muscles of shoulder internal
rotation and adduction (mean follow-up of 35.8
months). Another study107 of 104 patients (mean age
± SD = 21.5 ± 8.5 years) reported a success rate of
83% with a 6-week graduated exercise regime of limited
abduction (mean follow-up of 156 months).
These studies support a role for activity restriction
and exercise rehabilitation in the nonoperative management
of primary traumatic anterior shoulder dislocation.
In a prospective randomized study54 involving 40
patients, aged 30 years or younger, with a primary
traumatic anterior shoulder dislocation, Kirkley et
al54 reported a 47% redislocation rate for a treatment
group that received 3 weeks of immobilization
followed by a supervised shoulder range of motion
and muscle strengthening regime (activity restriction
enforced for 4 months). In the same study, a
redislocation rate of 16% was reported for a treatment
group that received immediate arthroscopic
surgery followed by an identical immobilization and
rehabilitation regime (mean follow-up of 32
months). Another prospective study17 involving 29
shoulders with recurrent anterior shoulder instability
secondary to a previous dislocation demonstrated
good or excellent results (as determined by the
Rowe and Zarins grading system84) in only 7% of
cases with a rehabilitation program that emphasized
progressive strengthening of the rotator cuff, deltoid,
and scapular stabilizer muscles (mean follow-up of 46
months). Further research is warranted to clarify the
efficacy of exercise rehabilitation in the nonoperative
management of primary traumatic anterior shoulder
dislocation.
Atraumatic Instability As for traumatic instability,
there have been few investigations pertaining to exercise
rehabilitation in the nonoperative management
of atraumatic shoulder instability. In a prospective
study17 of 47 patients (age range 12 to 54 years) with
anterior, posterior, and multidirectional instability of
atraumatic origin, good or excellent results as determined
by the Rowe and Zarins grading system84 were
reported in 80% of cases with a rehabilitation program
that emphasized progressive strengthening of
the rotator cuff, deltoid, and scapular stabilizer
muscles (mean follow-up of 46 months). Shoulder
strengthening and coordination exercises combined
with lifestyle modification is the most commonly recommended
treatment for atraumatic instability.
17,60,70,103
There is much to learn about the best methods to
enhance compression of the humeral head on the
glenoid and to restore scapulothoracic motion symmetry
and proprioception to the unstable shoulder.
Most authors have acknowledged the importance of
strengthening exercises for all components of the
rotator cuff and deltoid as a means of controlling
glenohumeral translation. Infraspinatus and teres
minor strengthening exercises performed in higher
degrees of abduction have been advocated as a
means for reducing anterior glenohumeral ligamentous
strain during the throwing motion.18 Strengthening
exercises have also been advocated for the biceps
brachii as well as the latissimus dorsi, pectoralis
major, and teres major to enhance the stabilizing
action of the rotator cuff muscles at the
glenohumeral joint.27,46,78,104
Functional exercises that require coordination
among multiple muscle groups (eg, hitting a tennis
ball backhanded) have been recommended for retraining
normal patterns of muscle activity in the
patient with shoulder instability.27 In a pilot project80
involving nonoperative treatment of atraumatic anterior
shoulder instability, significant improvements in
work and sport function and pain intensity were reported
for a functional retraining program designed
to improve rotator cuff muscle control through the use of electromyographic biofeedback. Changes in
work and sport function and pain intensity were not
significant for a second rehabilitation program that
consisted of isokinetic resistance exercises designed
to improve shoulder muscle strength and endurance.
Various forms of scapular muscle retraining have
been advocated in the rehabilitation of shoulder instability.
27,53,105 These have included exercises designed
to stabilize the scapulothoracic articulation
(isometric exercises, manual stabilization techniques),
to restore normal patterns of scapular
muscle activity (upper extremity weight-bearing activities),
and to maximize scapulothoracic muscle
strength and endurance in preparation for a return
to normal functional use (resistance exercises,
plyometric exercises, sport-specific drills). It remains
to be determined whether scapular motion asymmetry
can be corrected with exercise rehabilitation in
the patient with shoulder instability.
The interplay between neural and muscular
mechanisms for dynamic glenohumeral joint stability
is incompletely understood. Inman45 theorized that
proprioceptive mechanisms were elicited as a result
of specific movement patterns rather than isolated
muscle actions. This theory would imply a role for
functional exercises that include positions of instability
to evoke reflexive muscular activity that may protect
against potential joint instability. Other forms of
neuromuscular re-education,27,104,105,106 including
joint repositioning tasks, proprioceptive
neuromuscular facilitation techniques, upper extremity
weight-bearing exercises, and plyometric exercises
have been used to retrain proprioceptive mechanisms.
Further research is needed to determine the
efficacy of these exercises in the rehabilitation of
shoulder instability.
Surgical Management
Traumatic Unidirectional Instability The most recent
and most successful surgical procedures for unidirectional
shoulder instability reattach the detached
labrum and associated glenohumeral ligaments with
little disruption to the length or attachment of other
structures around the shoulder (Bankart repair). An
open Bankart repair consists of detachment and later
reattachment of the humeral insertion of subscapularis
(or a split of the subscapularis) and a reattachment
of the labrum to the anterior glenoid with sutures
through bone or with suture anchors. Most
surgeons also reduce any capsular redundancy by
tightening the anterior capsule with sutures. Open
anterior stabilization is associated with a 12° loss of
external rotation of the shoulder, probably secondary
to shortening of the subscapularis tendon after
detachment-reattachment.34
Arthroscopic techniques for unidirectional
glenohumeral instability have been developed to reattach
the labrum without an open incision and without
subscapularis detachment. The reported
redislocation rates for arthroscopic anterior shoulder
stabilization are higher than those reported for open
procedures (2–18% versus 11%) (Table 1). However,
arthroscopic procedures are associated with less loss
in external rotation than open procedures.
Arthroscopic techniques for reattaching the labrum
can be divided into three categories: (1) a
transglenoid suture technique,14,26,35,51,62,74,76 (2)
arthroscopically delivered and tied suture anchors,
33,40,93 and (3) arthroscopically delivered biodegradable
tacs.4,12,25,26,28,51,52,86,92 A comparison of the
reported rates of recurrent dislocation for each technique
is made in the Table.
Multidirectional Instability The most commonly performed
and most successfully reported surgical procedure
for multidirectional instability of the shoulder
is an anterior capsular shift, an open procedure that
involves the overlaying and thus shortening of the
anterior and inferior capsule.3,60,77 Closure of the
capsular interval between the subscapularis and
supraspinatus has been reported to be successful in a
small series of patients with subluxation.30,36
More recently, capsular shrinkage has been advocated
as a treatment for more subtle cases of shoulder
instability. Thermal denaturation of collagen results
in uncoupling of the triple helices and
shortening of the collagen. A recent study noted a
15% to 40% reduction in length of a cadaveric
shoulder capsule subjected to 65°C to 72°C heat
(Figure 5).98 Also noted was an associated 15% loss
in load to failure properties. Arthroscopic devices
have been designed to deliver heat to the shoulder
capsule with the potential to ‘‘shrink’’ redundant
capsule arthroscopically. A short-term study has reported
excellent results using this technique.86 Further
long-term evaluations are necessary to identify
the technique, indications, and results of this novel
method of reducing capsular volume.
Postoperative Rehabilitation
The basic principles of nonoperative rehabilitation
for shoulder instability (restoration of glenohumeral
compression stability, scapulohumeral motion
synchrony, and proprioceptive mechanisms) apply
equally to postoperative patients. The specific content
of postoperative rehabilitation varies according
to the stabilization procedure performed, individual
pathology, and the activity level of the individual.
Anterior Stabilization
Cryotherapy Cryotherapy in the postoperative shoulder
(applied for 15-minute durations every 1 to 2 waking hours for the first 24 hours, and 4 to 6 times
daily for the ensuing 9 days) has been shown to significantly
decrease the frequency and intensity of
shoulder pain both at rest and during rehabilitation
as compared to no-cryotherapy conditions.91 We recommend
15 minutes of cryotherapy every second
hour for the first week after a stabilization procedure
and after every exercise session for the duration of
rehabilitation.
Activity Restriction The postoperative management
of anterior instability has typically involved a minimum
of 6 weeks of activity restriction to minimize
stress to healing structures. During this period of
limited upper extremity use, we recommend active
exercise of noninvolved joints (elbow, wrist, and
hand). In the case of the injured athlete, rehabilitation
also aims to maintain cardiovascular fitness and
lower limb and trunk muscle condition.
Isometric Exercise Isometric shoulder muscle exercises,
initially performed with the arm adducted by
the side of the body, provide a means for preventing
muscular inhibition during the period of activity restriction.
Isometric exercises for the scapulothoracic
muscles are commenced during the first postoperative
week. Isometric exercises for the humeral muscles are commenced during the second postoperative
week. Care is taken when performing isometric
internal rotation for the first 6 weeks following an
open Bankart repair, in which the subscapularis
muscle is detached and reattached, to prevent rupture
from its humeral insertion. We recommend
pain-free contractions of 3 to 5 seconds duration and
a minimum of 30 daily repetitions20,32,64 for all isometric
exercises.
Range of Motion Exercises Assisted shoulder exercises
initially performed within a limited range of motion
are designed to protect the surgical repair and prevent
adhesion formation in the early postoperative
period. These exercises are commenced during the
second postoperative week. External rotation range
of motion is limited to 30° (0° abduction) for the
first 4 postoperative weeks. Combined external rotation
and abduction range of motion is avoided for
the first 6 postoperative weeks. Assisted elevation is
initially performed in the plane of the scapula to
maximize humeral and glenoid congruency.50 The
absence of pain, apprehension, and abnormal movement
patterns with assisted exercise are prerequisite
for the progression to active range of motion exercise.
Rehabilitation aims to restore full active range
of motion by 12 weeks after arthroscopic29 and open
anterior stabilization.103
Scapulothoracic Muscle Retraining In addition to isometric
scapulothoracic muscle exercises, the first
postoperative week involves treatment for any
strength or flexibility deficits within the lumbar or
thoracic areas.53 Upper extremity weight-bearing exercises
that incorporate specific scapular movements
at glenohumeral angles of less than 60° elevation are
introduced during the third postoperative week.53
Light resistance exercises are commenced during the
fourth postoperative week. We emphasize retraining
for scapular protraction and retraction and advocate
multiple sets of up to 30 repetitions for exercises
that involve both concentric and eccentric modes of
contraction.
Dynamic scapulothoracic stability, scapulohumeral
motion synchrony, and an absence of pain and apprehension
for movements performed between 0°
and 90° elevation are prerequisite for further rehabilitation
progression. Once these goals have been
achieved, upper extremity weight-bearing exercises
are advanced to higher angles of elevation and
weight-bearing loads are increased (eg, press-ups,
push-ups, and quadruped exercises).53 The
scapulothoracic muscles are comprehensively conditioned
through the use of free weights,27,67 various
resistance machines27,53 (eg, rowing, upright rows,
and pull-downs, anterior to the frontal plane) and
training activities27,105,106 (eg, throwing movement
exercises, blocking and ball defense exercises, and
water-based exercises) designed to replicate stresses
that will be imposed upon the shoulder during functional
upper extremity use.
Rotator Cuff and Humeral Muscle Strengthening Exercises
Rotator cuff strengthening is commenced with
isometric exercises, as detailed above. Light resistance
exercises for the rotator cuff and biceps
brachii muscles are introduced during the fourth
postoperative week. (For open stabilization procedures
involving detachment or reattachment of the
subscapularis, resistance exercises for the
subscapularis muscle are introduced during the sixth
postoperative week). We advocate exercises that involve
both concentric and eccentric modes of contraction
initially performed at glenohumeral angles
of less than 45° elevation. We use the same range of
motion to commence strengthening of the latissimus
dorsi, pectoralis major, and teres major.
Dynamic control of the scapulothoracic and
glenohumeral joints and an absence of pain and apprehension
for movements performed between 0°
and 45° elevation are prerequisite for exercise progression
to higher angles of elevation. Rotator cuff
strengthening for higher angles of elevation includes
the use of Theraband27,105 (eg, internal and external
rotation), free weights11,49,94 (eg, prone horizontal
abduction with arm externally rotated and scapular
plane elevation), and training activities27,106 (eg, underarm,
side-arm, and overhead throwing or catching
exercises using balls of various weights and sizes).
Humeral muscle strengthening includes Theraband
exercises27 (eg, extension and adduction initiated
from 90° flexion and abduction, respectively), free
weights94 (scapular plane elevation with arm internally
rotated and horizontal abduction with arm internally
and externally rotated), press-ups,27,94 pushups,
48 and various weight machines.27
Proprioception In the latter stage of rehabilitation,
emphasis is given to functional exercises that prepare
the neuromuscular and cardiovascular systems for
the return to sports participation. We include activities
that require the coordination of multiple
muscles (eg, catching and throwing activities, racquet
and other batting activities, and goal defense activities)
to achieve the desired magnitude, duration, and
sequence of motor output for a given functional
task. These exercises initially use glenohumeral positions
that are least likely to provoke an instability
episode. An absence of symptoms and quality of
movement are fundamental prerequisites for exercise
progression to positions that maximally challenge the
dynamic shoulder restraints.
Stabilization for Multidirectional Instability: Special
Considerations
Postoperative rehabilitation for multidirectional
instability is characterized by activity restriction and
strict range of motion control. Care is taken to pre-vent overstretching of tightened capsular tissues, particularly
after thermal shrinkage procedures that induce
an initial decrease in collagen tensile
strength.95,98 We restrict axial loading of the upper
extremity for 6 weeks. For cases with an anterior
component of instability, we restrict external rotation
range of motion to 30° (0° abduction) for the first
4 postoperative weeks and avoid combined external
rotation and abduction range of motion for the first
6 postoperative weeks. For cases with a posterior
component of instability, we avoid combined flexion,
internal rotation, and horizontal adduction for the
first 6 postoperative weeks.
Glenohumeral and scapulothoracic muscle retraining
guidelines used in the postoperative management
of anterior instability are also appropriate for the
postoperative rehabilitation of multidirectional instability.
We advocate a more conservative approach to
the rate of rehabilitation progression after stabilization
procedure for multidirectional instability, as the
success of this condition may be more dependent
upon the restoration of normal shoulder muscle
function.
CONCLUSION
In summary, there have been significant advances
in methods to restore function in both unidirectional
and multidirectional shoulder instability.68
Biomechanical and anatomical studies have enhanced
our understanding of the mechanics of the
shoulder joint with implications for the management
and rehabilitation of shoulder instability. Further investigation
of the mechanisms responsible for dynamic
glenohumeral control will help to delineate
the optimal treatment for shoulder instability.